Bcbs Botox Prior Authorization Form
Bcbs Botox Prior Authorization Form - Web for drugs that require prior authorization, providers should submit requests as follows: Blue cross commercial medicare plus blue sm blue. Print the form and mail to: Web medication authorization request forms for drugs covered under the medical benefit on this page you'll find information for: Web blue cross and blue shield of kansas attention: Blue cross and blue shield of. Please contact the member’s primary coverage for determination of benefit and additional information. Web drug specific prior authorization form prescription drug claim form texas standard prior authorization request form for prescription drug benefits find a doctor or. Botox j0585 / dysport j0586 / xeomin j0588 / myobloc j0587. For pharmacy benefit drugs, submit requests through covermymeds.
Botox j0585 / dysport j0586 / xeomin j0588 / myobloc j0587. Botox® dysport® myobloc® xeomin® check one: Blue cross commercial medicare plus blue sm blue. Web if secondary, an authorization is not needed through this process. Providers have the opportunity to request the method to receive their prior authorization (pa) exemption communications*. Web ask your provider to go to prior authorization requests to get forms and information on services that may need approval before they prescribe a specific medicine, medical. For pharmacy benefit drugs, submit requests through covermymeds. Web drug specific prior authorization form prescription drug claim form texas standard prior authorization request form for prescription drug benefits find a doctor or. Print the form and mail to: Web blue cross and blue shield of kansas attention:
Print the form and mail to: Blue cross commercial medicare plus blue sm blue. Please contact the member’s primary coverage for determination of benefit and additional information. Web prior authorization botulinum toxin. 12/09/2021 botox® (onabotulinumtoxina) dysport® (abobotulinumtoxina) xeomin® (incobotulinumtoxina) hcpcs: Web blue cross and blue shield of kansas attention: Providers have the opportunity to request the method to receive their prior authorization (pa) exemption communications*. Botox® dysport® myobloc® xeomin® check one: Web prior review (prior plan approval, prior authorization, prospective review or certification) is the process bcbsnc uses to review the provision of certain medical services and. Web effective may 1, 2019, blue cross and blue shield of minnesota and blue plus (blue cross) providers are required to use the availity® provider portal to submit preservice.
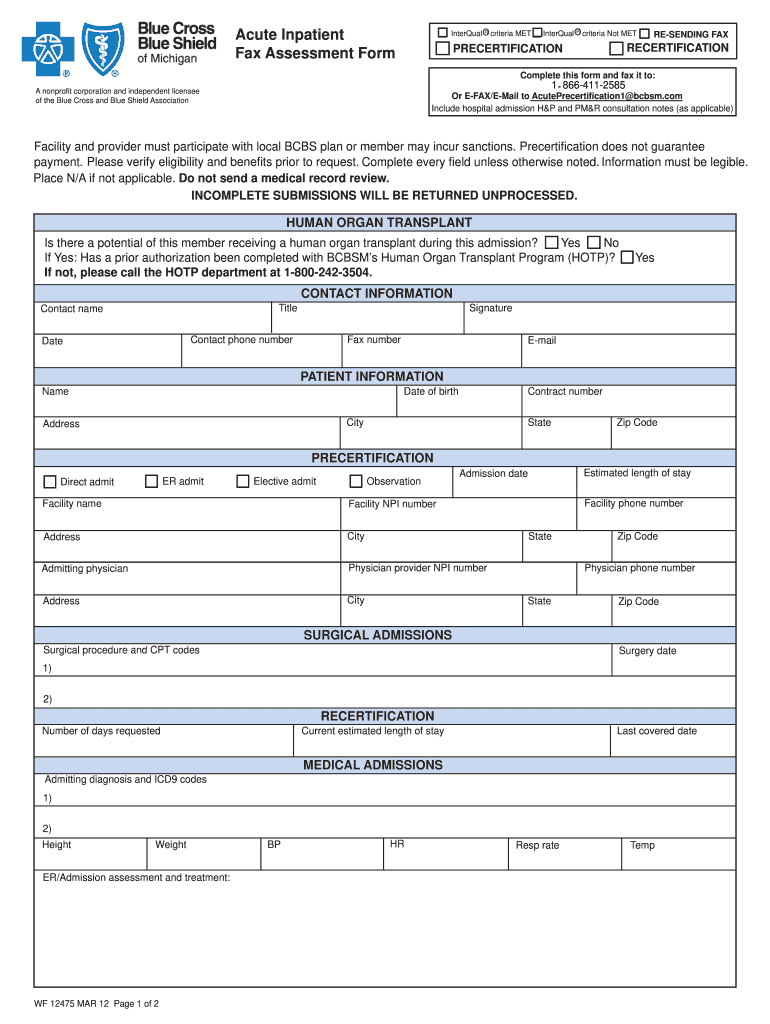
2012 MI BCBS Acute Inpatient Assessment Form Fill Online, Printable
Maximum allowable cost (mac) appeal form. Web if secondary, an authorization is not needed through this process. Botox® dysport® myobloc® xeomin® check one: 12/09/2021 botox® (onabotulinumtoxina) dysport® (abobotulinumtoxina) xeomin® (incobotulinumtoxina) hcpcs: The preferred pa form for government programs products is located on providers.bluecrossmn.com.
Bcbs Prior Authorization Form Medication Form Resume Examples
The preferred pa form for government programs products is located on providers.bluecrossmn.com. For pharmacy benefit drugs, submit requests through covermymeds. Web botox (onabotulinum toxin a) dysport (abobotulinum toxin a) myobloc (rimabotulinum toxin b) xeomin (incobotulinum toxin a) botox (onabotulinum toxin a) will be approved when. Web medication authorization request forms for drugs covered under the medical benefit on this page.
Highmark Bcbs Medication Prior Authorization form Inspirational Billing
12/09/2021 botox® (onabotulinumtoxina) dysport® (abobotulinumtoxina) xeomin® (incobotulinumtoxina) hcpcs: The preferred pa form for government programs products is located on providers.bluecrossmn.com. Web follow these steps to submit prior authorization requests when prescribing drugs covered under the medical benefit for blue cross blue shield of michigan and blue care. Blue cross and blue shield of. Web if secondary, an authorization is not.
Bcbs Prior Authorization Form Tennessee Form Resume Examples
Web if secondary, an authorization is not needed through this process. Web botox (onabotulinum toxin a) dysport (abobotulinum toxin a) myobloc (rimabotulinum toxin b) xeomin (incobotulinum toxin a) botox (onabotulinum toxin a) will be approved when. Web follow these steps to submit prior authorization requests when prescribing drugs covered under the medical benefit for blue cross blue shield of michigan.
Anthem BCBS 490773 2015 Fill and Sign Printable Template Online US
The preferred pa form for government programs products is located on providers.bluecrossmn.com. Web for drugs that require prior authorization, providers should submit requests as follows: Web prior review (prior plan approval, prior authorization, prospective review or certification) is the process bcbsnc uses to review the provision of certain medical services and. Web if secondary, an authorization is not needed through.
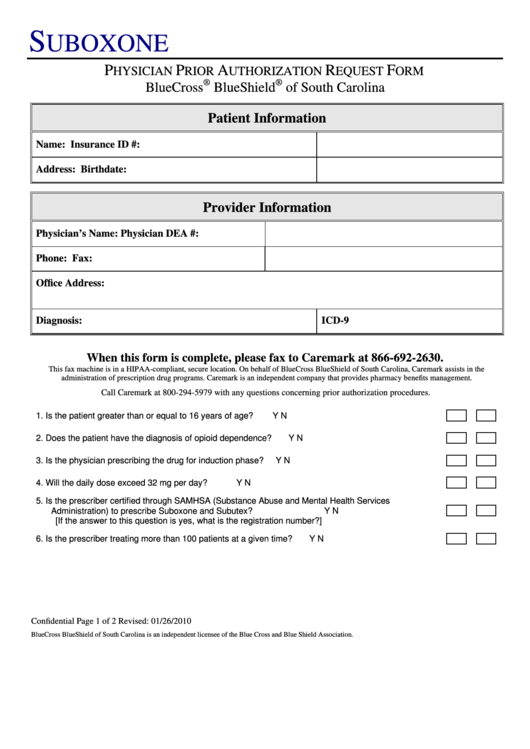
Bcbs Suboxone Physician Prior Authorization Request Form printable pdf
Web if secondary, an authorization is not needed through this process. Web prior authorization botulinum toxin. For pharmacy benefit drugs, submit requests through covermymeds. Botox® dysport® myobloc® xeomin® check one: 12/09/2021 botox® (onabotulinumtoxina) dysport® (abobotulinumtoxina) xeomin® (incobotulinumtoxina) hcpcs:
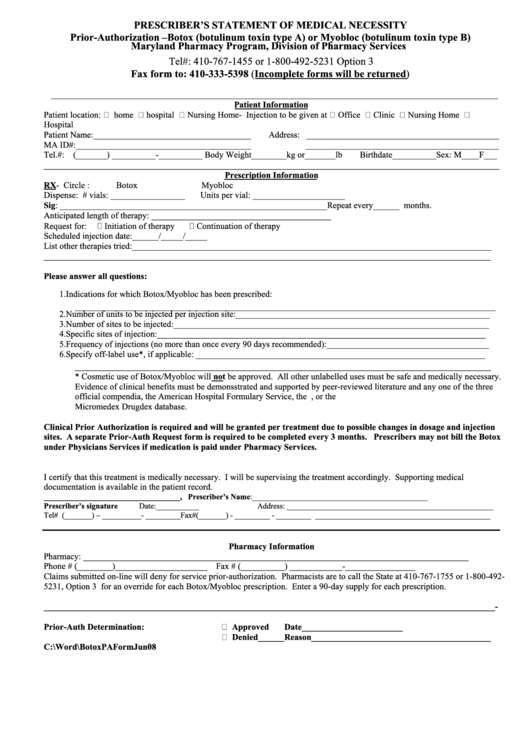
Botox Or Myobioc Prior Authorization Form Prescriber'S Statement Of
Web medication authorization request forms for drugs covered under the medical benefit on this page you'll find information for: Blue cross and blue shield of. Web drug specific prior authorization form prescription drug claim form texas standard prior authorization request form for prescription drug benefits find a doctor or. Botox® dysport® myobloc® xeomin® check one: Web botox (onabotulinum toxin a).
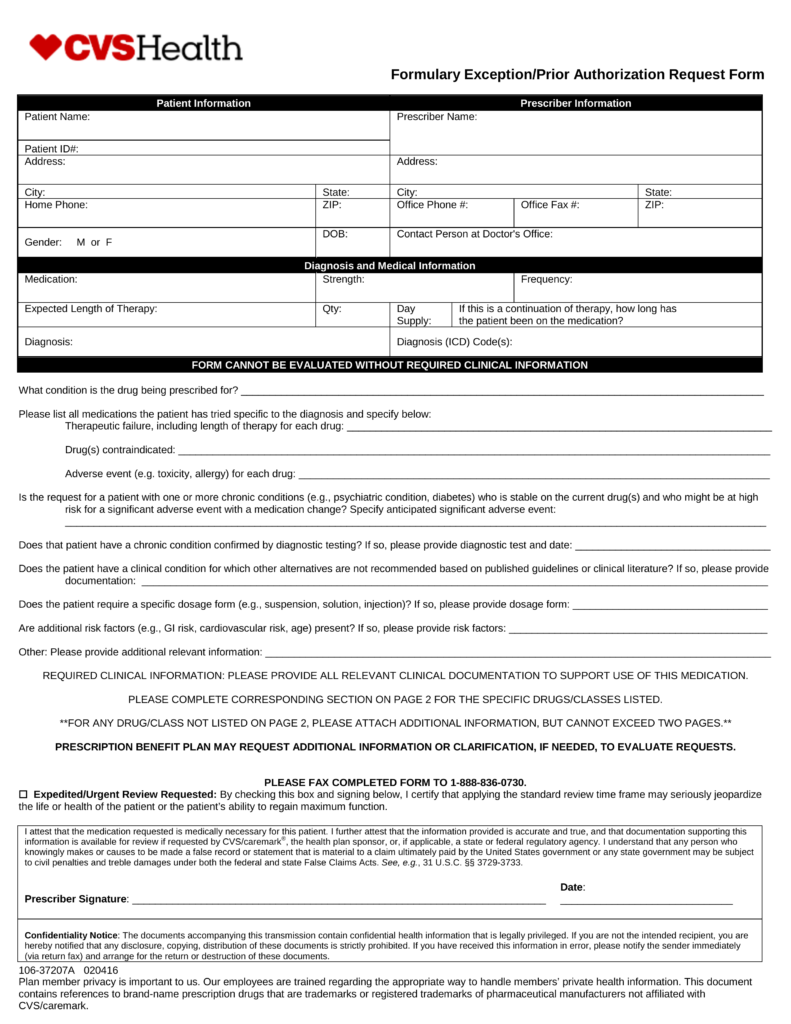
Free CVS/Caremark Prior (Rx) Authorization Form PDF eForms
Print the form and mail to: Web botox (onabotulinum toxin a) dysport (abobotulinum toxin a) myobloc (rimabotulinum toxin b) xeomin (incobotulinum toxin a) botox (onabotulinum toxin a) will be approved when. Blue cross commercial medicare plus blue sm blue. Blue cross and blue shield of. Web effective may 1, 2019, blue cross and blue shield of minnesota and blue plus.
Bcbs Prior Auth Form Texas Form Resume Examples pA8MQOk8Ra
Web pharmacy utilization management programs. Please contact the member’s primary coverage for determination of benefit and additional information. Web follow these steps to submit prior authorization requests when prescribing drugs covered under the medical benefit for blue cross blue shield of michigan and blue care. The preferred pa form for government programs products is located on providers.bluecrossmn.com. Web blue cross.
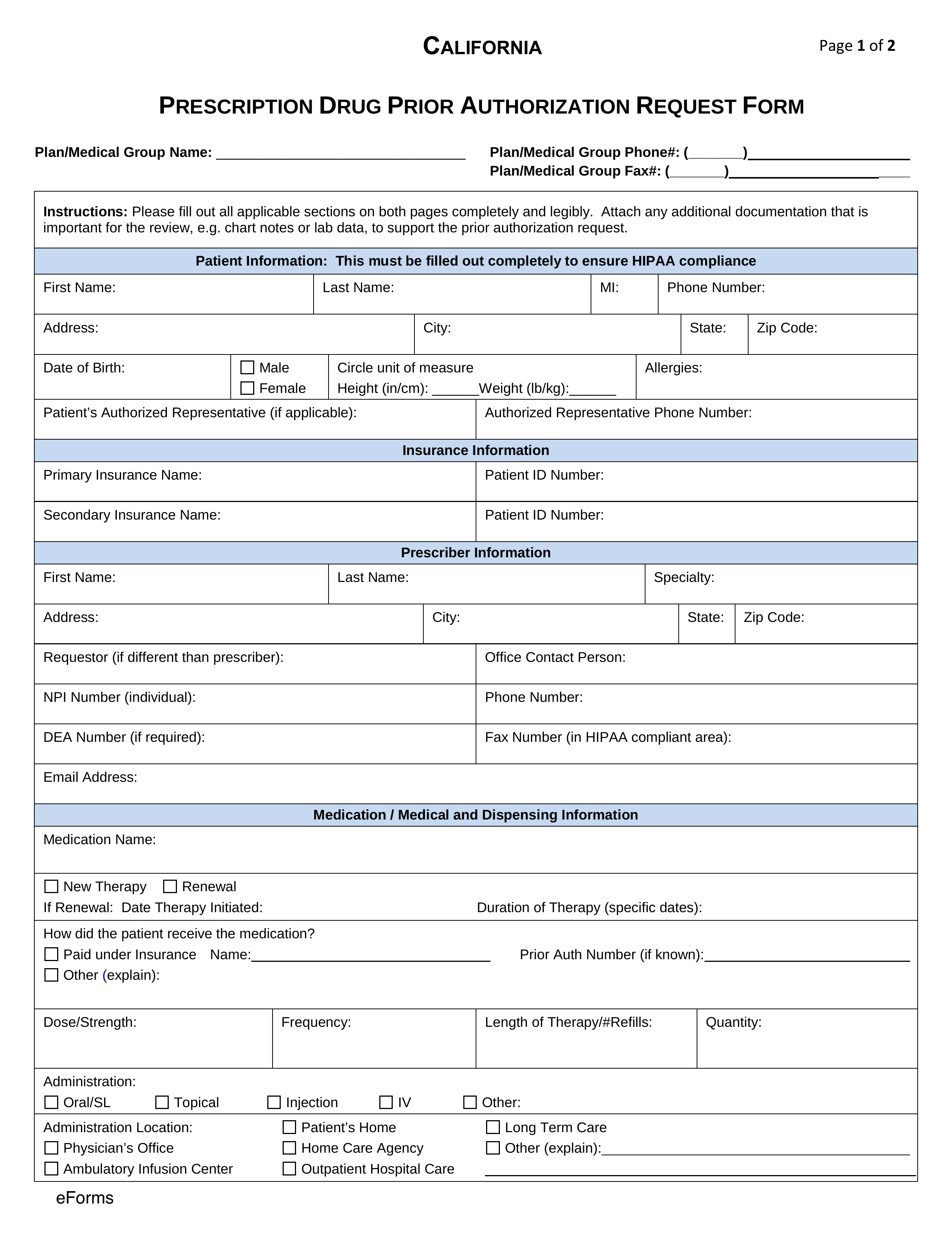
Free California Medicaid Prior (Rx) Authorization Form PDF eForms
Web blue cross and blue shield of kansas attention: Please contact the member’s primary coverage for determination of benefit and additional information. Web if secondary, an authorization is not needed through this process. Web prior authorization botulinum toxin. If you have questions regarding the prior authorization, please contact cvs caremark at 1.
Web If Secondary, An Authorization Is Not Needed Through This Process.
Web medication authorization request forms for drugs covered under the medical benefit on this page you'll find information for: Web effective may 1, 2019, blue cross and blue shield of minnesota and blue plus (blue cross) providers are required to use the availity® provider portal to submit preservice. Web drug specific prior authorization form prescription drug claim form texas standard prior authorization request form for prescription drug benefits find a doctor or. Web effective may 1, 2019, blue cross and blue shield of minnesota and blue plus (blue cross) providers are required to use the availity® provider portal to submit preservice prior.
The Preferred Pa Form For Government Programs Products Is Located On Providers.bluecrossmn.com.
Blue cross commercial medicare plus blue sm blue. Web follow these steps to submit prior authorization requests when prescribing drugs covered under the medical benefit for blue cross blue shield of michigan and blue care. Botox® dysport® myobloc® xeomin® check one: Providers have the opportunity to request the method to receive their prior authorization (pa) exemption communications*.
Web Pharmacy Utilization Management Programs.
Web for drugs that require prior authorization, providers should submit requests as follows: Web prior review (prior plan approval, prior authorization, prospective review or certification) is the process bcbsnc uses to review the provision of certain medical services and. 12/09/2021 botox® (onabotulinumtoxina) dysport® (abobotulinumtoxina) xeomin® (incobotulinumtoxina) hcpcs: Please contact the member’s primary coverage for determination of benefit and additional information.
Print The Form And Mail To:
Web blue cross and blue shield of kansas attention: Blue cross and blue shield of. Web botox (onabotulinum toxin a) dysport (abobotulinum toxin a) myobloc (rimabotulinum toxin b) xeomin (incobotulinum toxin a) botox (onabotulinum toxin a) will be approved when. If you have questions regarding the prior authorization, please contact cvs caremark at 1.