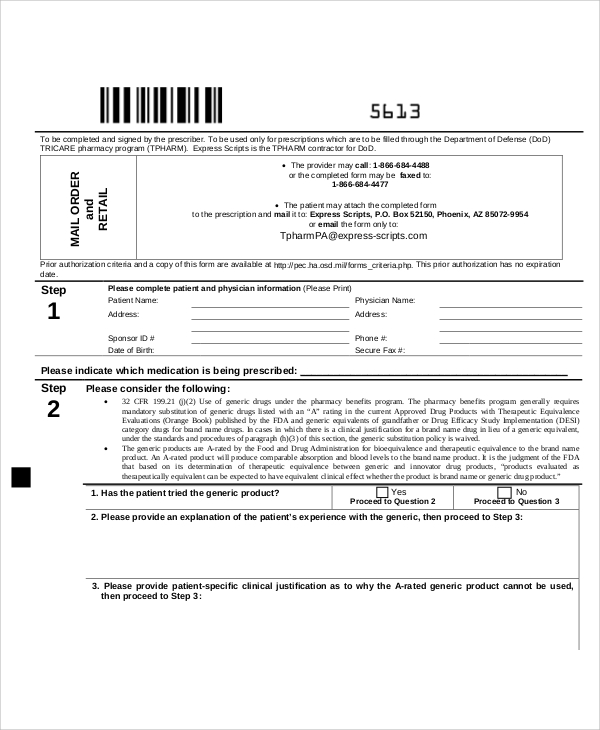
Express Scripts Medication Prior Auth Form
Express Scripts Medication Prior Auth Form - Web prior authorization form medicare coverage determination and redetermination to initiate the coverage review process or an appeal of a previously declined coverage review. Web *some plans might not accept this form for medicare or medicaid requests. Web certain medications may need approval from your insurance carrier before they are covered. Find tricare claims forms, our medical questionnaire, and. Web how to get medical necessity. Be in writing and signed, state specifically why you disagree, include a copy of the claim decision, and; Web prior authorization drug forms phone: ☐ ☐initial request continuation/renewal request reason. Select the appropriate express scripts form to get started. This form is being used for:
Give the form to your provider to complete and send back to express scripts. Download and print the form for your drug. Select the appropriate express scripts form to get started. Be in writing and signed, state specifically why you disagree, include a copy of the claim decision, and; A prior authorization form must be submitted if the prescribed medication. To read information, use the down arrow from a form field. Web register now we make it easy to share information get your written prescriptions to us by using our mail order form. Web how to get medical necessity. This form is being used for: Web express scripts resources for pharmacists.
A prior authorization form must be submitted if the prescribed medication. Read latest notifications, file pricing appeals and search express scripts claims and patient coverage for your pharmacy customers. Web how to get medical necessity. Give the form to your provider to complete and send back to express scripts. Web register now we make it easy to share information get your written prescriptions to us by using our mail order form. To read information, use the down arrow from a form field. Web *some plans might not accept this form for medicare or medicaid requests. Download and print the form for your drug. This form is being used for: Be in writing and signed, state specifically why you disagree, include a copy of the claim decision, and;
Gallery of Highmark Bcbs Medication Prior Authorization form Best Of
To read information, use the down arrow from a form field. Find tricare claims forms, our medical questionnaire, and. ☐ ☐initial request continuation/renewal request reason. Read latest notifications, file pricing appeals and search express scripts claims and patient coverage for your pharmacy customers. Download and print the form for your drug.
Express Scripts Prior Authorization Form Medicare Part D Form
Web prior authorization form medicare coverage determination and redetermination to initiate the coverage review process or an appeal of a previously declined coverage review. Find tricare claims forms, our medical questionnaire, and. ☐ ☐initial request continuation/renewal request reason. Download and print the form for your drug. Read latest notifications, file pricing appeals and search express scripts claims and patient coverage.
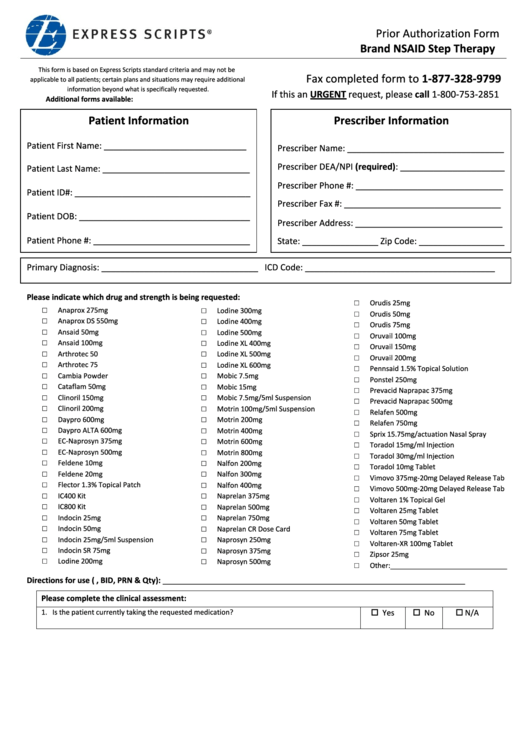
Express Scripts Prior Authorization Form Brand Nsaid Step Therapy
Web portal allowing you manage prescription drug epas for patients with express scripts pharmacy benefits, either if your patient’s physical plan is part of attention continue. Give the form to your provider to complete and send back to express scripts. Web a to the prescription and mail it to: Web prior authorization form medicare coverage determination and redetermination to initiate.
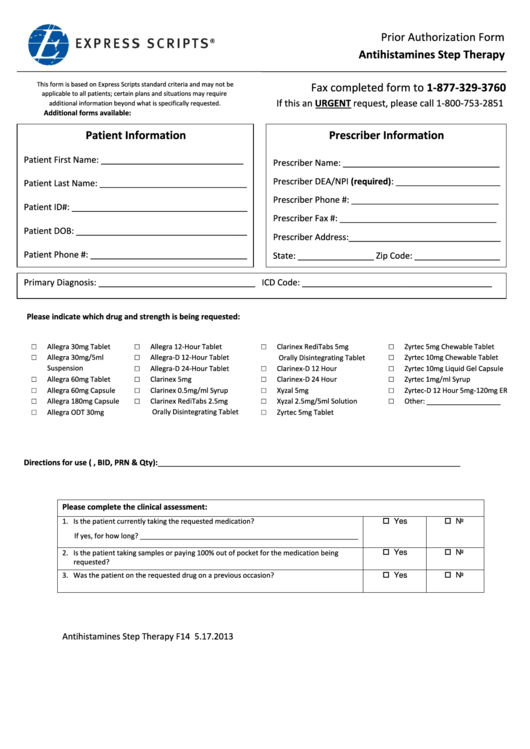
Express Scripts Prior Authorization Form Antihistamines Step Therapy
This form is being used for: Web certain medications may need approval from your insurance carrier before they are covered. Web prior authorization form medicare coverage determination and redetermination to initiate the coverage review process or an appeal of a previously declined coverage review. Web *some plans might not accept this form for medicare or medicaid requests. To read information,.
Gallery of Highmark Bcbs Medication Prior Authorization form Best Of
Web express scripts has partnered with covermymeds to offer electronic prior authorization (epa) services. This form is being used for: A prior authorization form must be submitted if the prescribed medication. Read latest notifications, file pricing appeals and search express scripts claims and patient coverage for your pharmacy customers. To read information, use the down arrow from a form field.
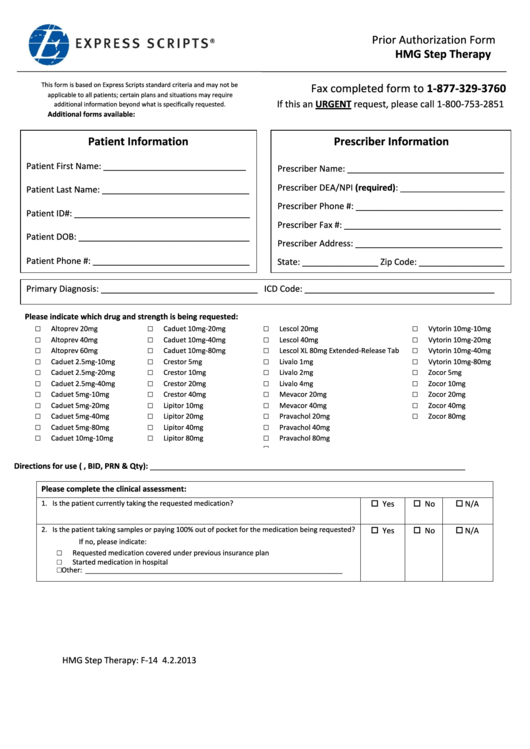
Express Scripts Prior Authorization Form Hmg Step Therapy printable
Web portal allowing you manage prescription drug epas for patients with express scripts pharmacy benefits, either if your patient’s physical plan is part of attention continue. Web register now we make it easy to share information get your written prescriptions to us by using our mail order form. Web request for prior authorization this document contains both information and form.
Gallery of Highmark Bcbs Medication Prior Authorization form Lovely
☐ ☐initial request continuation/renewal request reason. Web a to the prescription and mail it to: Web portal allowing you manage prescription drug epas for patients with express scripts pharmacy benefits, either if your patient’s physical plan is part of attention continue. Web *some plans might not accept this form for medicare or medicaid requests. Be in writing and signed, state.
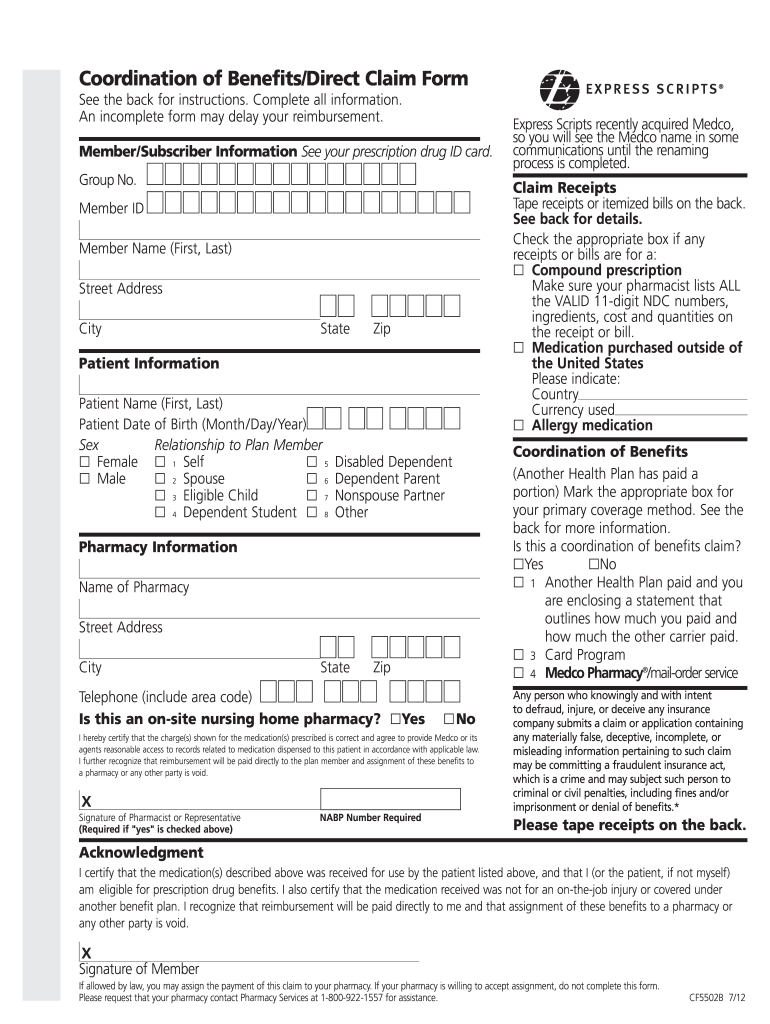
Free Express Scripts Prior (Rx) Authorization Form PDF eForms
Web request for prior authorization this document contains both information and form fields. Web prior authorization form medicare coverage determination and redetermination to initiate the coverage review process or an appeal of a previously declined coverage review. To read information, use the down arrow from a form field. Download and print the form for your drug. ☐ ☐initial request continuation/renewal.
Express Scripts Appeal Form Fill Out and Sign Printable PDF Template
Web prior authorization drug forms phone: Web request for prior authorization this document contains both information and form fields. Web prior authorization form medicare coverage determination and redetermination to initiate the coverage review process or an appeal of a previously declined coverage review. Download and print the form for your drug. Find tricare claims forms, our medical questionnaire, and.
FREE 10+ Sample Authorization Request Forms in MS Word PDF
To read information, use the down arrow from a form field. Download and print the form for your drug. A prior authorization form must be submitted if the prescribed medication. This form is being used for: Web prior authorization form medicare coverage determination and redetermination to initiate the coverage review process or an appeal of a previously declined coverage review.
Web Express Scripts Resources For Pharmacists.
This form is being used for: Web prior authorization drug forms phone: Web request for prior authorization this document contains both information and form fields. Download and print the form for your drug.
Web Portal Allowing You Manage Prescription Drug Epas For Patients With Express Scripts Pharmacy Benefits, Either If Your Patient’s Physical Plan Is Part Of Attention Continue.
To read information, use the down arrow from a form field. Find tricare claims forms, our medical questionnaire, and. Read latest notifications, file pricing appeals and search express scripts claims and patient coverage for your pharmacy customers. Web register now we make it easy to share information get your written prescriptions to us by using our mail order form.
Web Express Scripts Has Partnered With Covermymeds To Offer Electronic Prior Authorization (Epa) Services.
Web certain medications may need approval from your insurance carrier before they are covered. Web *some plans might not accept this form for medicare or medicaid requests. Web prior authorization form medicare coverage determination and redetermination to initiate the coverage review process or an appeal of a previously declined coverage review. Be in writing and signed, state specifically why you disagree, include a copy of the claim decision, and;
A Prior Authorization Form Must Be Submitted If The Prescribed Medication.
☐ ☐initial request continuation/renewal request reason. Give the form to your provider to complete and send back to express scripts. Select the appropriate express scripts form to get started. Web how to get medical necessity.