Molina Auth Form
Molina Auth Form - 2023 medicaid pa guide/request form (vendors) effective 07.01.2023 important information for molina healthcare medicaid providers information generally required to support authorization decision making includes: All medications are listed by generic name. • current (up to 6 months), adequate patient history related to the requested. 2021 prior authorization guide/request form effective 08.01.21. Texas standardized prior authorization request form for healthcare services. Web prior authorization is when your provider gets approval from molina healthcare to provide you a service. Please enter all the mandatory fields for the form to be submitted please select captcha. Molina healthcare of south carolina, inc. The medications are organized by therapeutic classes. Web molina® healthcare, inc.
Prior authorization is not a guarantee of payment for services. Behavioral health service request form. • current (up to 6 months), adequate patient history related to the requested. It is needed before you can get certain services or drugs. If prior authorization is needed for a certain service, your provider must get it before giving you the service. 2023 medicaid pa guide/request form (vendors) effective 07.01.2023 important information for molina healthcare medicaid providers information generally required to support authorization decision making includes: See what sets us apart. Web molina has provided the best healthcare quality and affordability for more than 30 years. Please enter all the mandatory fields for the form to be submitted please select captcha. Web the molina healthcare drug formulary is a listing of preferred drug products eligible for reimbursement by molina healthcare.
Q1 2022 medicare pa guide/request form effective 01.01.2021 phone: Please enter all the mandatory fields for the form to be submitted please select captcha. Web molina has provided the best healthcare quality and affordability for more than 30 years. Pharmacy and outpatient drug services. For questions or comments about your coverage, or. • current (up to 6 months), adequate patient history related to the requested. All medications are listed by generic name. The medications are organized by therapeutic classes. Texas standardized prior authorization request form for healthcare services. 2023 medicaid pa guide/request form (vendors) effective 07.01.2023 important information for molina healthcare medicaid providers information generally required to support authorization decision making includes:
WA Molina Healthcare Behavioral Health Authorization/Notification Form
Web molina® healthcare, inc. Prior authorization is not a guarantee of payment for services. If prior authorization is needed for a certain service, your provider must get it before giving you the service. It is needed before you can get certain services or drugs. • current (up to 6 months), adequate patient history related to the requested.
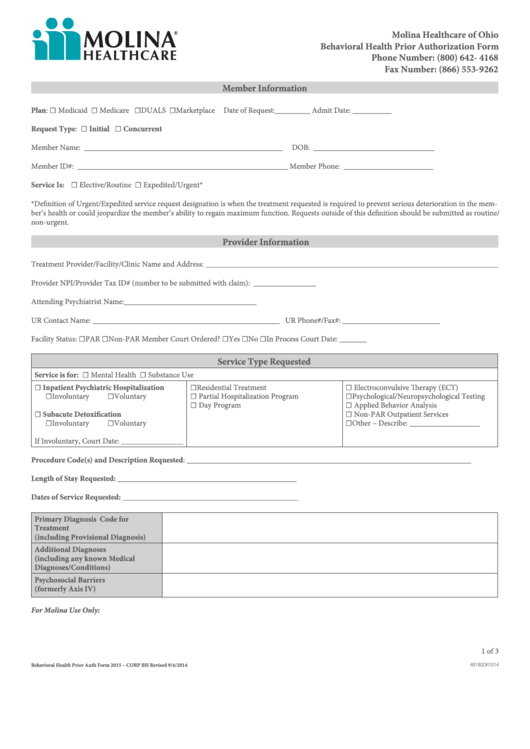
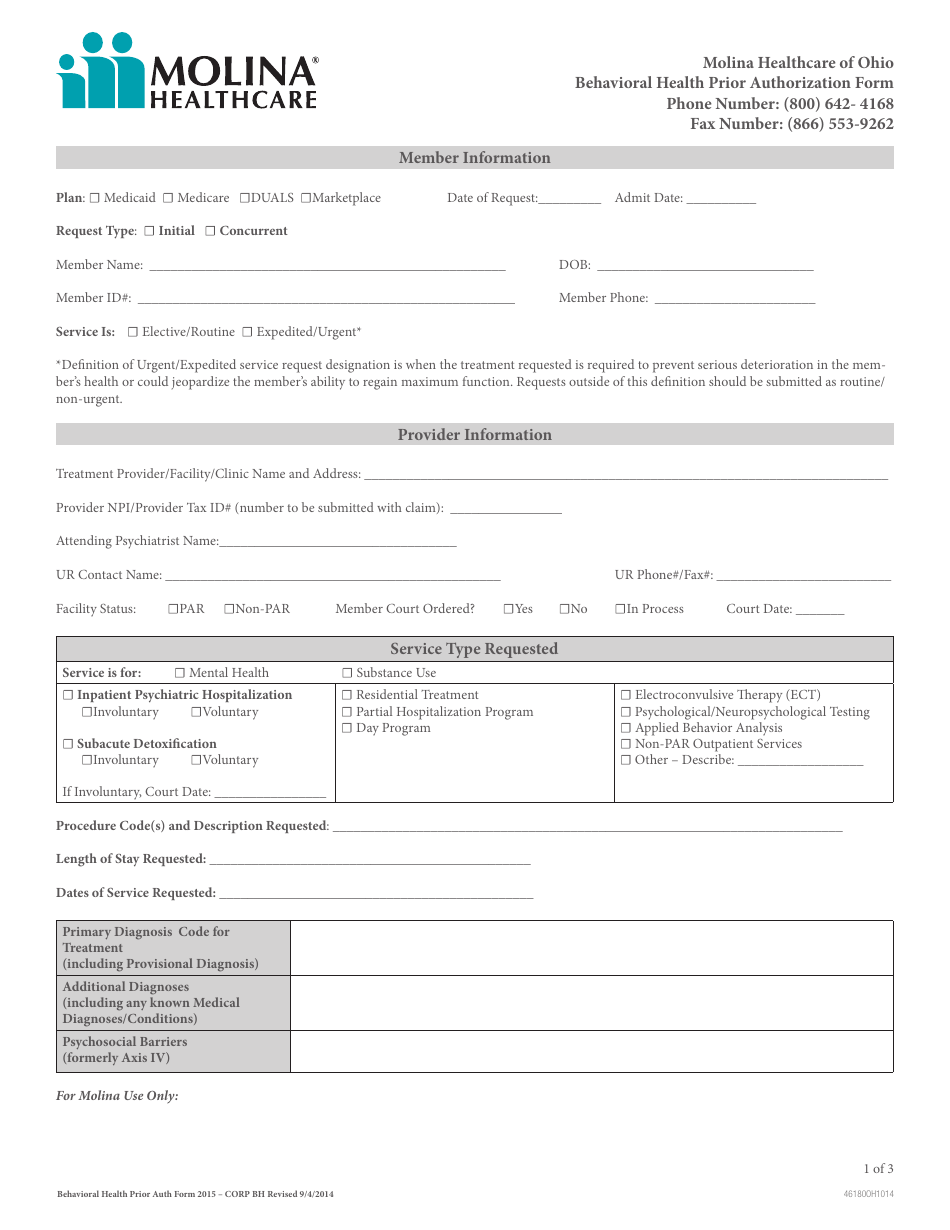
Fillable Molina Behavioral Health Prior Authorization Form Ohio
The medications are organized by therapeutic classes. Q1 2022 medicare pa guide/request form effective 01.01.2021 phone: Texas standardized prior authorization request form for healthcare services. • current (up to 6 months), adequate patient history related to the requested. Web prior authorization is when your provider gets approval from molina healthcare to provide you a service.
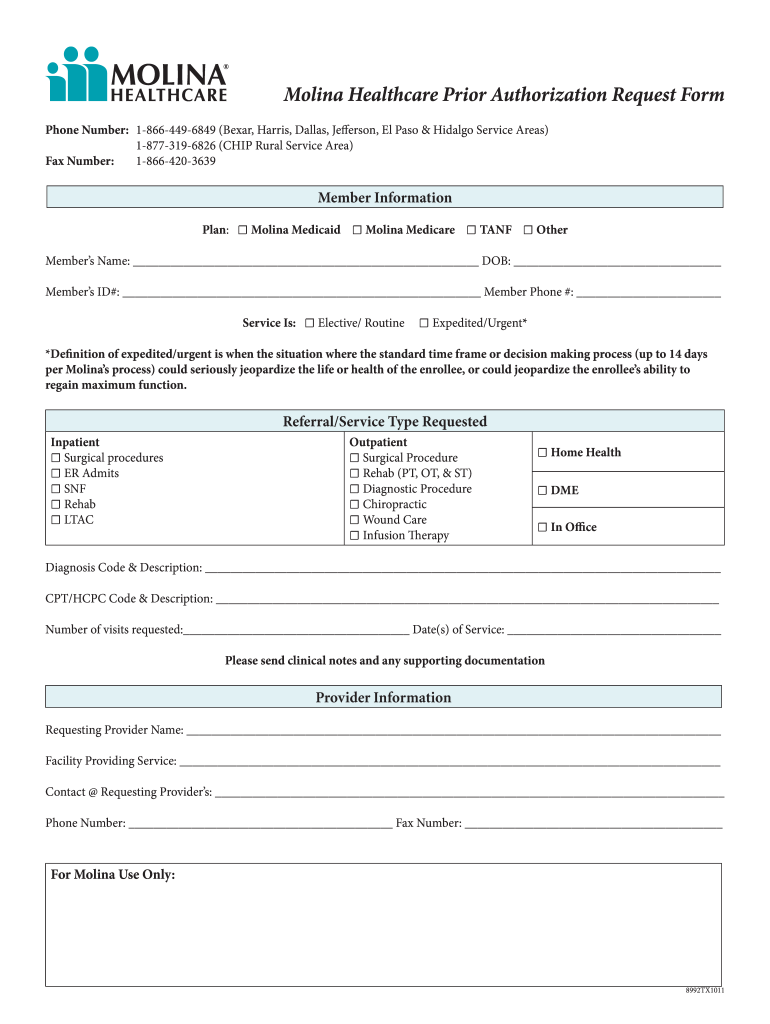
Molina Prior Authorization Form 2021 Fill Online, Printable, Fillable
Q1 2022 medicare pa guide/request form effective 01.01.2021 phone: Texas standardized prior authorization request form for healthcare services. See what sets us apart. If prior authorization is needed for a certain service, your provider must get it before giving you the service. Web molina has provided the best healthcare quality and affordability for more than 30 years.
Ohio Behavioral Health Prior Authorization Molina Healthcare Download
For questions or comments about your coverage, or. Web medicaid behavioral health and medical services prior authorization code matrix. It is needed before you can get certain services or drugs. Molina healthcare of south carolina, inc. Web prior authorization is when your provider gets approval from molina healthcare to provide you a service.
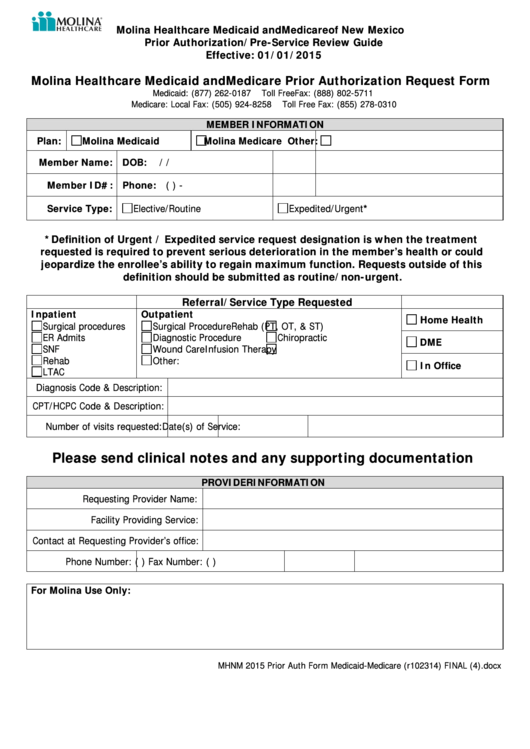
Molina Healthcare Medicaid And Medicare Prior Authorization Request
2023 medicaid pa guide/request form (vendors) effective 07.01.2023 important information for molina healthcare medicaid providers information generally required to support authorization decision making includes: It is needed before you can get certain services or drugs. 2021 prior authorization guide/request form effective 08.01.21. Web medicaid behavioral health and medical services prior authorization code matrix. Pharmacy and outpatient drug services.
Gallery of Molina Prior Authorization form 2018 Lovely why It is Not
Texas standardized prior authorization request form for healthcare services. The medications are organized by therapeutic classes. If prior authorization is needed for a certain service, your provider must get it before giving you the service. For questions or comments about your coverage, or. Web medicaid behavioral health and medical services prior authorization code matrix.
Molina Medicare Pa Forms Universal Network
All medications are listed by generic name. Behavioral health service request form. Molina healthcare of south carolina, inc. • current (up to 6 months), adequate patient history related to the requested. 2023 medicaid pa guide/request form (vendors) effective 07.01.2023 important information for molina healthcare medicaid providers information generally required to support authorization decision making includes:
Molina Medicare Medication Prior Authorization Form Form Resume
Web the molina healthcare drug formulary is a listing of preferred drug products eligible for reimbursement by molina healthcare. 2023 medicaid pa guide/request form (vendors) effective 07.01.2023 important information for molina healthcare medicaid providers information generally required to support authorization decision making includes: If prior authorization is needed for a certain service, your provider must get it before giving you.
Aarp Medicare Supplement Prior Authorization Form Form Resume
2023 medicaid pa guide/request form (vendors) effective 07.01.2023 important information for molina healthcare medicaid providers information generally required to support authorization decision making includes: • current (up to 6 months), adequate patient history related to the requested. 2021 prior authorization guide/request form effective 08.01.21. Please enter all the mandatory fields for the form to be submitted please select captcha. Web.
Gallery of Molina Prior Authorization form 2018 Beautiful Frontiers
Web medicaid behavioral health and medical services prior authorization code matrix. 2021 prior authorization guide/request form effective 08.01.21. 2023 medicaid pa guide/request form (vendors) effective 07.01.2023 important information for molina healthcare medicaid providers information generally required to support authorization decision making includes: All medications are listed by generic name. Behavioral health service request form.
Molina Healthcare Of South Carolina, Inc.
Prior authorization is not a guarantee of payment for services. The medications are organized by therapeutic classes. Web medicaid behavioral health and medical services prior authorization code matrix. Q1 2022 medicare pa guide/request form effective 01.01.2021 phone:
Please Enter All The Mandatory Fields For The Form To Be Submitted Please Select Captcha.
Behavioral health service request form. Texas standardized prior authorization request form for healthcare services. Web the molina healthcare drug formulary is a listing of preferred drug products eligible for reimbursement by molina healthcare. Web molina has provided the best healthcare quality and affordability for more than 30 years.
All Medications Are Listed By Generic Name.
Pharmacy and outpatient drug services. If prior authorization is needed for a certain service, your provider must get it before giving you the service. 2021 prior authorization guide/request form effective 08.01.21. For questions or comments about your coverage, or.
It Is Needed Before You Can Get Certain Services Or Drugs.
• current (up to 6 months), adequate patient history related to the requested. See what sets us apart. Web molina® healthcare, inc. Prescriptions for medications requiring prior approval or for medications not included on the molina healthcare drug.