Molina Credentialing Form
Molina Credentialing Form - Web pharmacy credentialing/recredentialing application completed forms can be sent to: Web ensure molina healthcare, inc. Is listed as an authorized plan to view your credentialing application caqh id #: Web credentialing contact (if different from above): Receive notification of the credentialing decision within 60 days of the committee decision; Prior authorization request contact information. By submitting my information via this form, i. ( ) name affiliated with tax id number: Web molina healthcare of ohio’s credentialing process is designed to meet the standards of the national committee for quality assurance (ncqa). Web find out if you can become a member of the molina family.
Web find out if you can become a member of the molina family. The practitioner must sign and date their. Practitioner application instructions complete all items as noted below and submit this application and attachments to your contracting. To avoid delays please ensure applications are current, including work. The application must be entirely complete. Web credentialing contact (if different from above): Providers date of birth (mm/dd/yy): Last four digits of ss#: Web the behavioral health special provider bulletin is a newsletter distributed by molina healthcare of ohio. Web molina healthcare prior authorization request form and instructions nursing facility request form synagis (rsv) authorization behavioral health respite services pa.
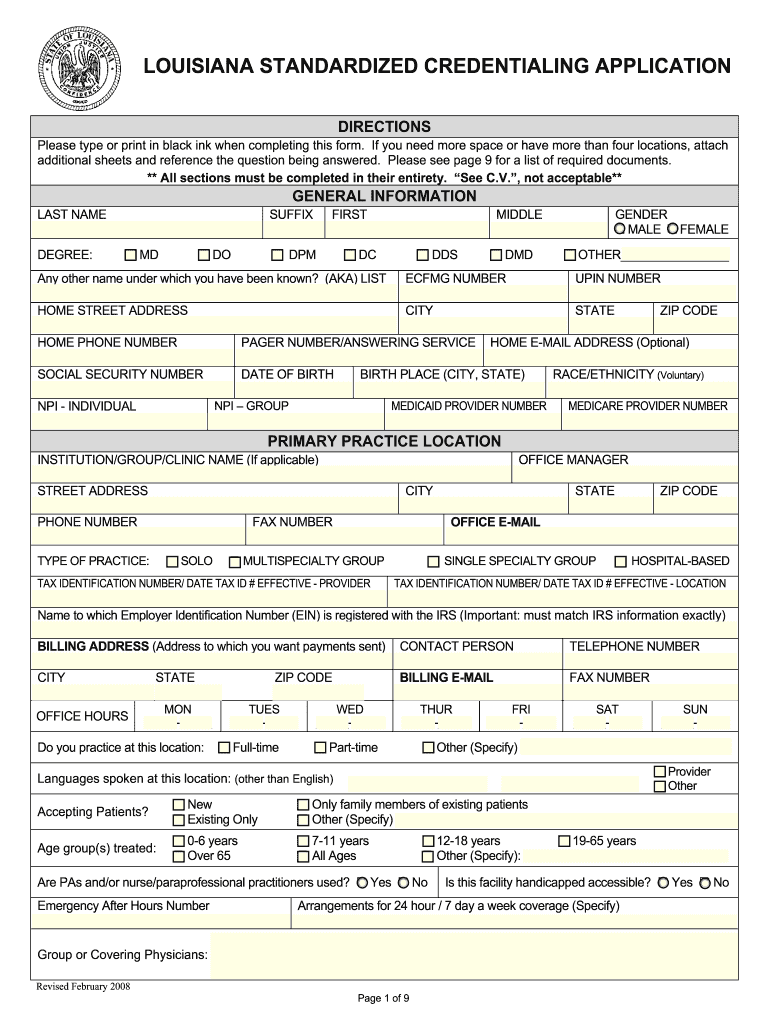
Receive notification of your rights as a provider to appeal. Providers date of birth (mm/dd/yy): Web washington law requires all health care providers submit credentialing applications through providersource. • a completed credentialing application, which includes but is not limited to: The application must be entirely complete. Receive notification of the credentialing decision within 60 days of the committee decision; Is listed as an authorized plan to view your credentialing application caqh id #: The practitioner must sign and date their. To join molina healthcare of mississippi's mississippican (medicaid) network, from july 1, 2022, you must be credentialed by the mississippi division of medicaid and. Web molina healthcare of ohio’s credentialing process is designed to meet the standards of the national committee for quality assurance (ncqa).
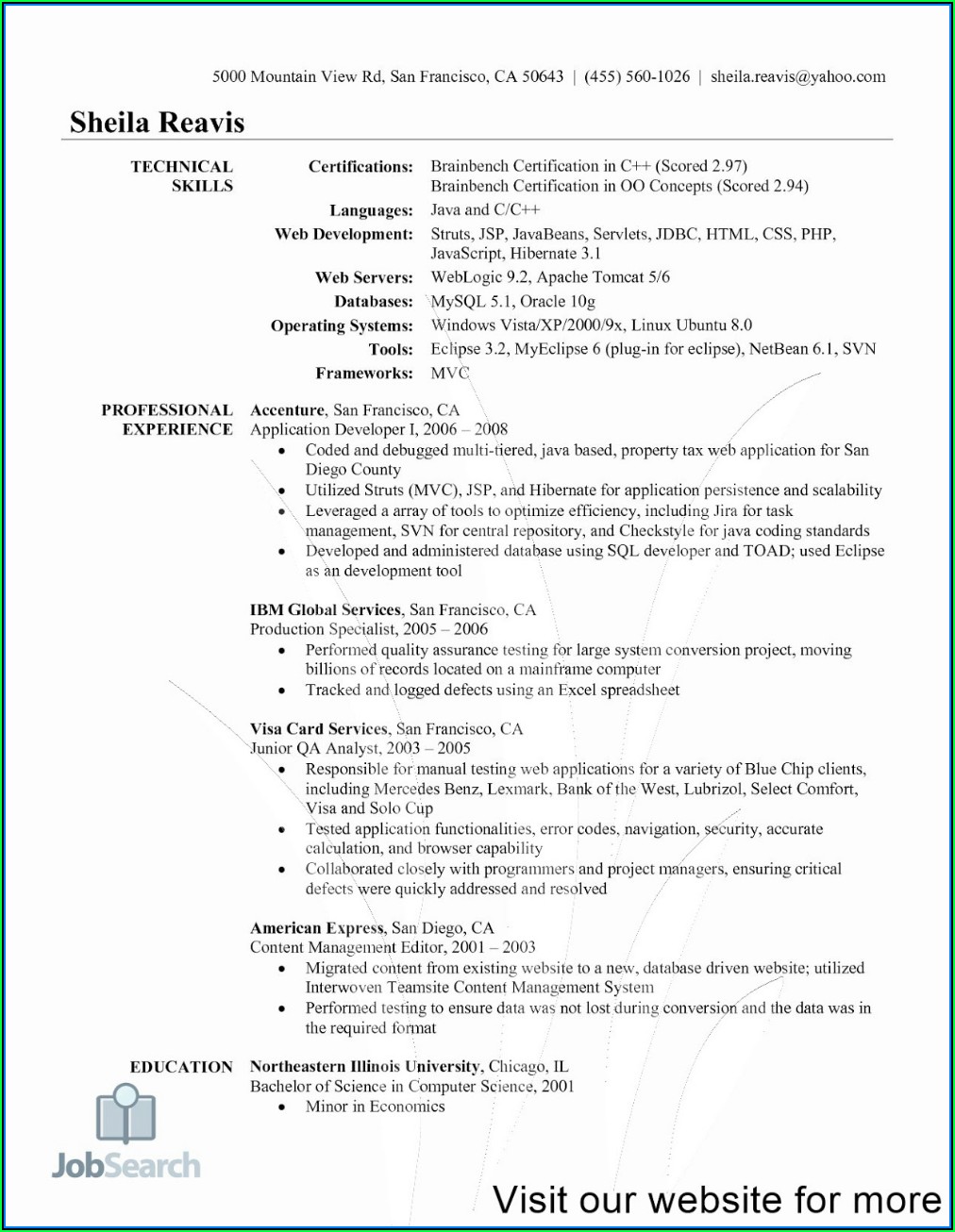
Molina Healthcare Credentialing Forms Form Resume Examples xz20pnnx2q
To avoid delays please ensure applications are current, including work. Is listed as an authorized plan to view your credentialing application caqh id #: To join molina healthcare of mississippi's mississippican (medicaid) network, from july 1, 2022, you must be credentialed by the mississippi division of medicaid and. Web molina healthcare prior authorization request form and instructions nursing facility request.
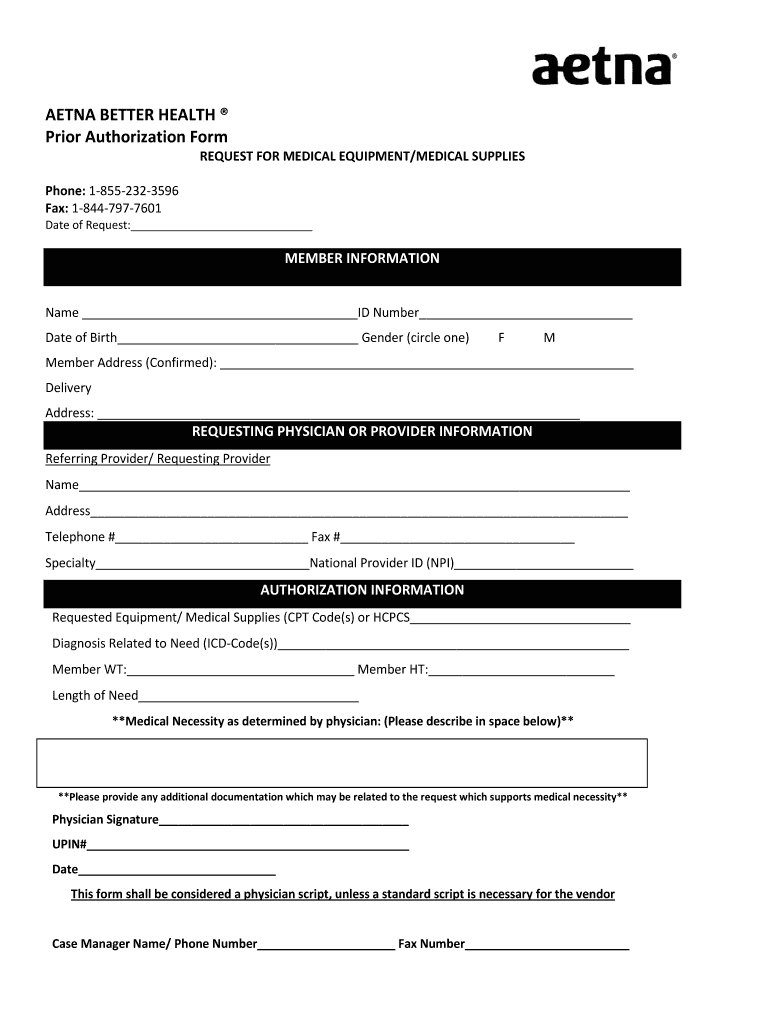
Aetna Better Health Prior Authorization Fill and Sign Printable
Practitioner application instructions complete all items as noted below and submit this application and attachments to your contracting. One protection is assurance that. Web pharmacy credentialing/recredentialing application completed forms can be sent to: Receive notification of the credentialing decision within 60 days of the committee decision; The practitioner must sign and date their.
Louisiana Standardized Credentialing Application Fill Out and Sign
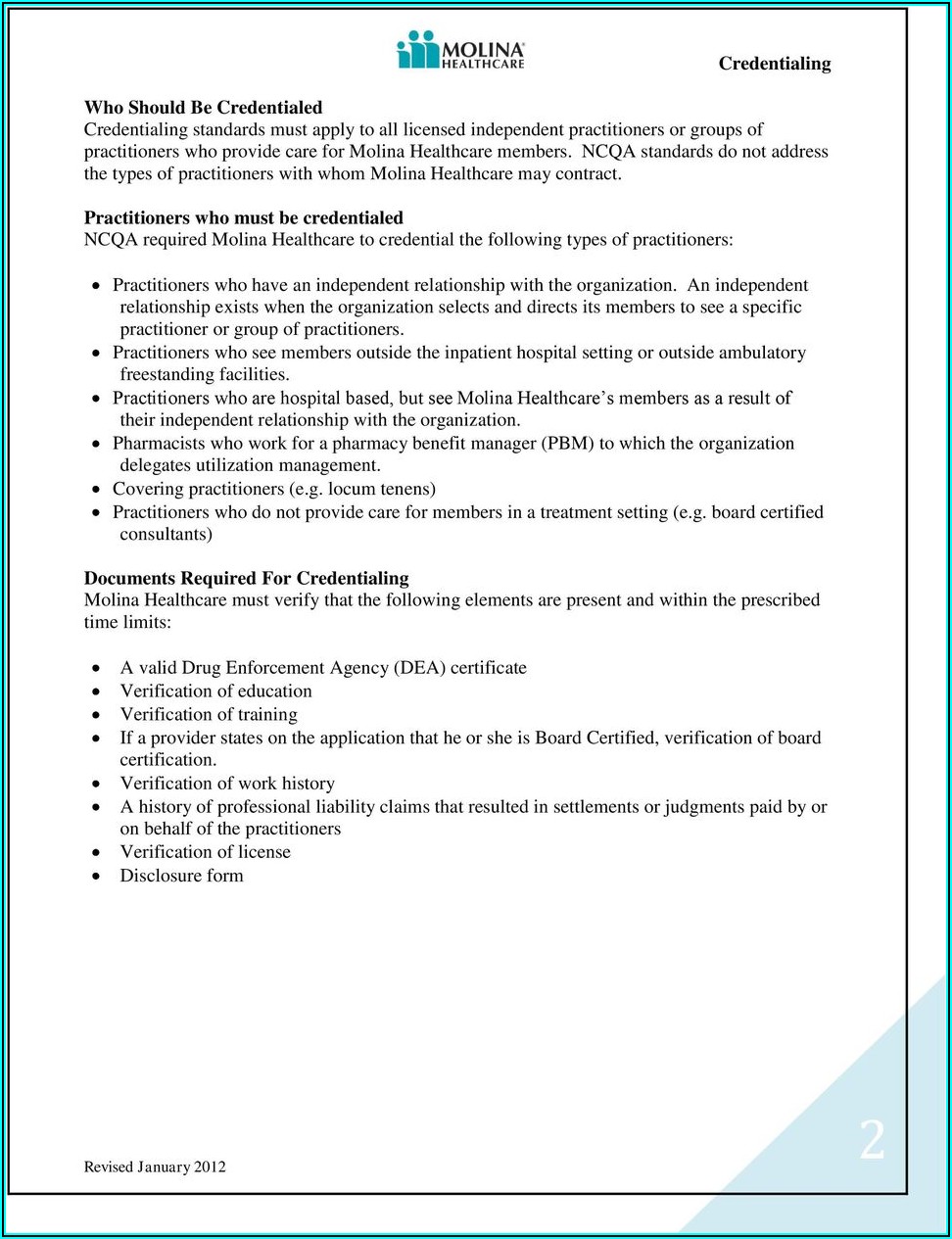
In accordance with those standards,. Pick your state and your preferred language to continue. Web credentialing molina healthcare has a duty to protect its members by assuring the care they receive is of the highest quality. Last four digits of ss#: Web molina healthcare of ohio’s credentialing process is designed to meet the standards of the national committee for quality.
Molina Healthcare Credentialing Forms Form Resume Examples xz20pnnx2q
To avoid delays please ensure applications are current, including work. Web find out if you can become a member of the molina family. Web washington law requires all health care providers submit credentialing applications through providersource. The practitioner must sign and date their. To join molina healthcare of mississippi's mississippican (medicaid) network, from july 1, 2022, you must be credentialed.
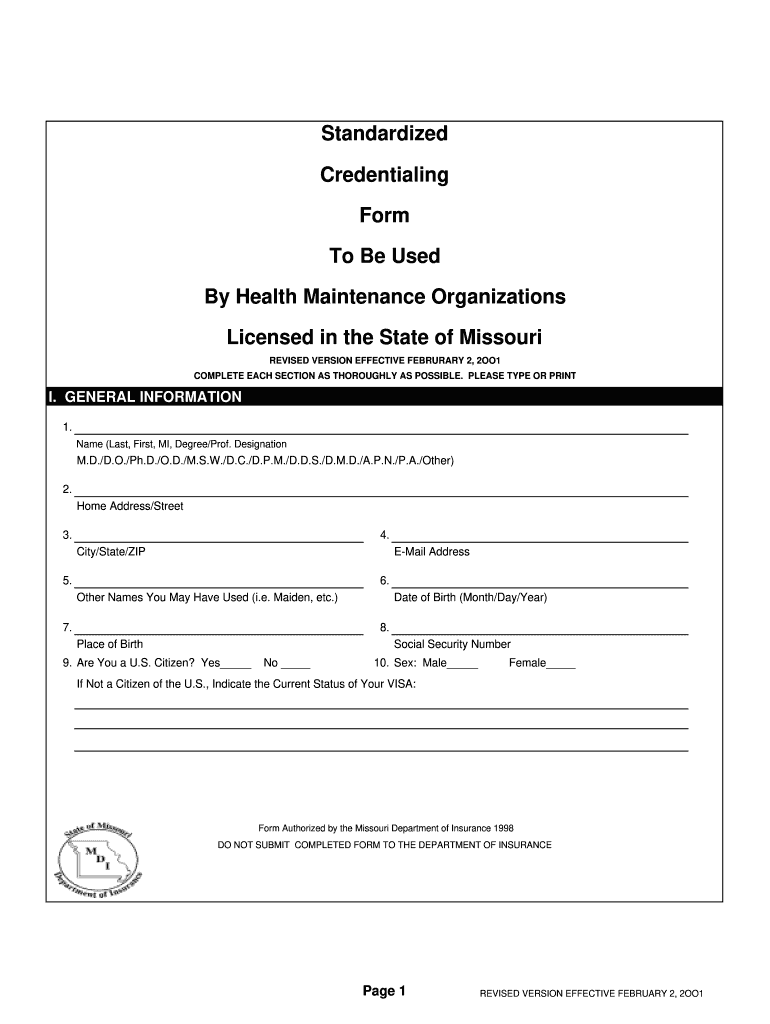
20012021 MO Standardized Credentialing Form Fill Online, Printable
Practitioner must complete and submit to molina a credentialing application. Web washington law requires all health care providers submit credentialing applications through providersource. Receive notification of your rights as a provider to appeal. Web ensure molina healthcare, inc. Web molina healthcare prior authorization request form and instructions nursing facility request form synagis (rsv) authorization behavioral health respite services pa.
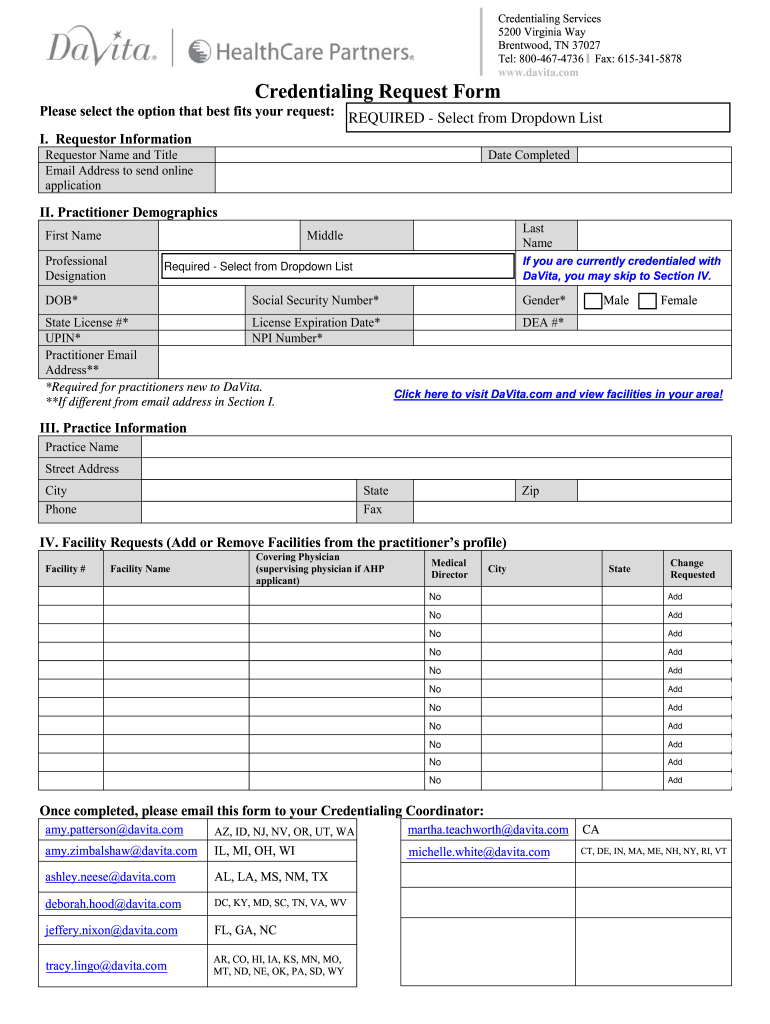
Credentialing Request Form Fill Out and Sign Printable PDF Template
Web pharmacy credentialing/recredentialing application completed forms can be sent to: Web the behavioral health special provider bulletin is a newsletter distributed by molina healthcare of ohio. Web credentialing contact (if different from above): Pick your state and your preferred language to continue. ( ) name affiliated with tax id number:
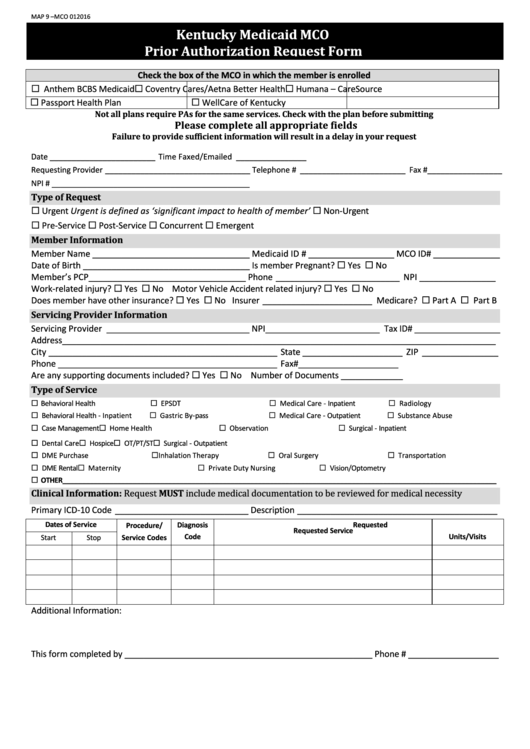
Fillable Kentucky Medicaid Mco Prior Authorization Request Form
Web ensure molina healthcare, inc. The practitioner must sign and date their. Practitioner must complete and submit to molina a credentialing application. Receive notification of your rights as a provider to appeal. To join molina healthcare of mississippi's mississippican (medicaid) network, from july 1, 2022, you must be credentialed by the mississippi division of medicaid and.
Molina Healthcare Credentialing Forms Form Resume Examples xz20pnnx2q
To avoid delays please ensure applications are current, including work. • a completed credentialing application, which includes but is not limited to: To join molina healthcare of mississippi's mississippican (medicaid) network, from july 1, 2022, you must be credentialed by the mississippi division of medicaid and. Receive notification of your rights as a provider to appeal. Web molina requirements for.
Form Standardized Credentialing Fill Online, Printable, Fillable
Web credentialing contact (if different from above): Web the behavioral health special provider bulletin is a newsletter distributed by molina healthcare of ohio. Receive notification of your rights as a provider to appeal. To avoid delays please ensure applications are current, including work. Web molina healthcare of ohio’s credentialing process is designed to meet the standards of the national committee.
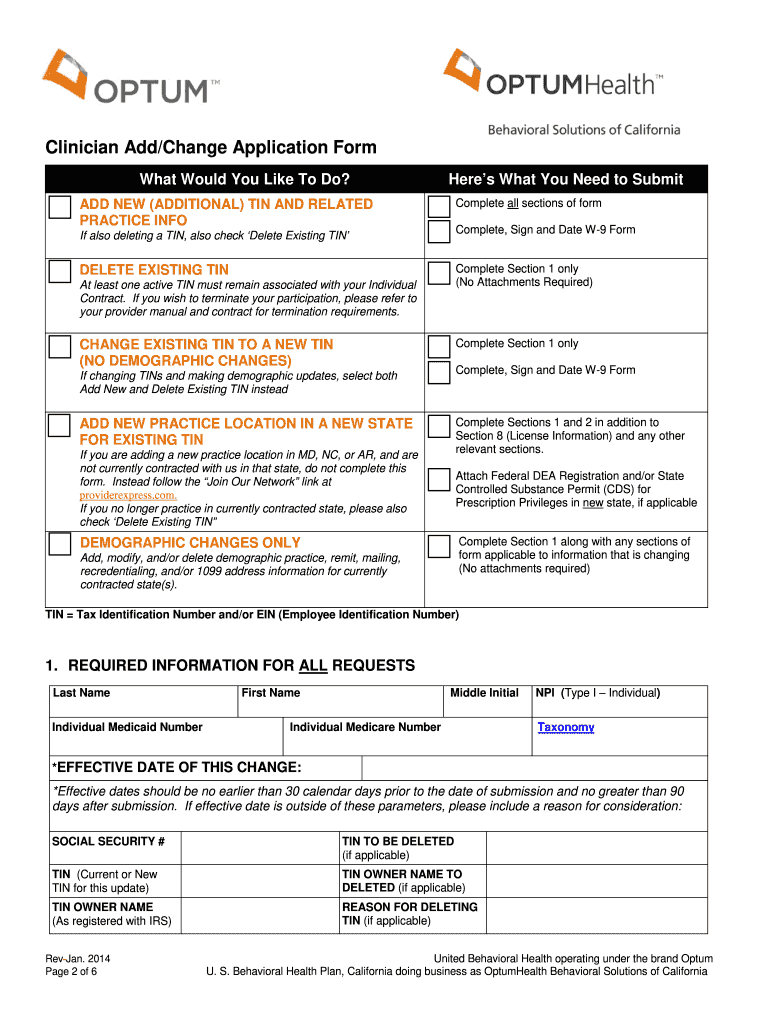
CA Clinician Add/Change Application Form 2014 Fill and Sign Printable
Receive notification of the credentialing decision within 60 days of the committee decision; Providers date of birth (mm/dd/yy): Web washington law requires all health care providers submit credentialing applications through providersource. Web credentialing molina healthcare has a duty to protect its members by assuring the care they receive is of the highest quality. ( ) name affiliated with tax id.
Last Four Digits Of Ss#:
Web washington law requires all health care providers submit credentialing applications through providersource. Pick your state and your preferred language to continue. Practitioner must complete and submit to molina a credentialing application. Web credentialing contact (if different from above):
Web The Behavioral Health Special Provider Bulletin Is A Newsletter Distributed By Molina Healthcare Of Ohio.
• a completed credentialing application, which includes but is not limited to: Web ensure molina healthcare, inc. Is listed as an authorized plan to view your credentialing application caqh id #: ( ) name affiliated with tax id number:
To Avoid Delays Please Ensure Applications Are Current, Including Work.
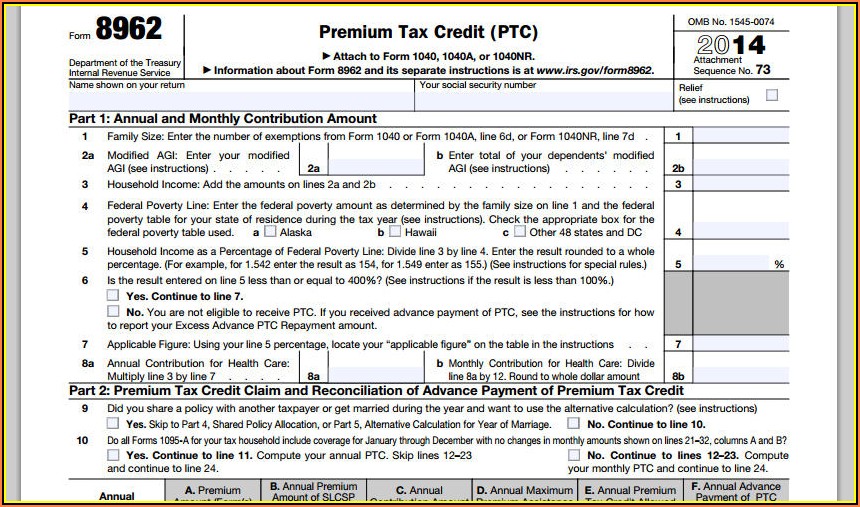
The application must be entirely complete. Providers date of birth (mm/dd/yy): By submitting my information via this form, i. Web molina healthcare prior authorization request form and instructions nursing facility request form synagis (rsv) authorization behavioral health respite services pa.
Receive Notification Of The Credentialing Decision Within 60 Days Of The Committee Decision;
Web credentialing molina healthcare has a duty to protect its members by assuring the care they receive is of the highest quality. Web find out if you can become a member of the molina family. Receive notification of your rights as a provider to appeal. Practitioner application instructions complete all items as noted below and submit this application and attachments to your contracting.