Molina Medicaid Authorization Form
Molina Medicaid Authorization Form - Web change office location, hours, phone, fax, or email. Add or terminate a provider. Open or close your practice to new patients ( pcps only ). Medicaid prior authorization annual review report. The fastest route for prior authorization is submission via fax. Prior authorization is when your provider gets approval from molina healthcare to provide you a service. Please use the “find a provider” tool above, which features pdf versions of our provider directories. Molina healthcare prior authorization request form and instructions. Items on this list will only be dispensed after prior authorization from molina healthcare. We’ve provided the following resources to help you understand molina’s authorization process and obtain authorization for your patients when required.
We’ve provided the following resources to help you understand molina’s authorization process and obtain authorization for your patients when required. Molina healthcare prior authorization request form and instructions. Add or terminate a provider. Change in tax id and/or npi. 2023 medicaid pa guide/request form (vendors) effective 07.01.2023 important information for molina healthcare medicaid providers information generally required to support authorization decision making includes: Prior authorization is when your provider gets approval from molina healthcare to provide you a service. Web change office location, hours, phone, fax, or email. Web getting care > prior authorizations prior authorizations what are prior authorizations? Open or close your practice to new patients ( pcps only ). Add or close a location.
The fastest route for prior authorization is submission via fax. • current (up to 6 months), adequate patient history related to the requested. Medicaid prior authorization annual review report. Open or close your practice to new patients ( pcps only ). Please use the “find a provider” tool above, which features pdf versions of our provider directories. Molina healthcare prior authorization request form and instructions. Add or close a location. Web change office location, hours, phone, fax, or email. 2023 medicaid pa guide/request form (vendors) effective 07.01.2023 important information for molina healthcare medicaid providers information generally required to support authorization decision making includes: Web health insurance can be complicated—especially when it comes to authorizations.
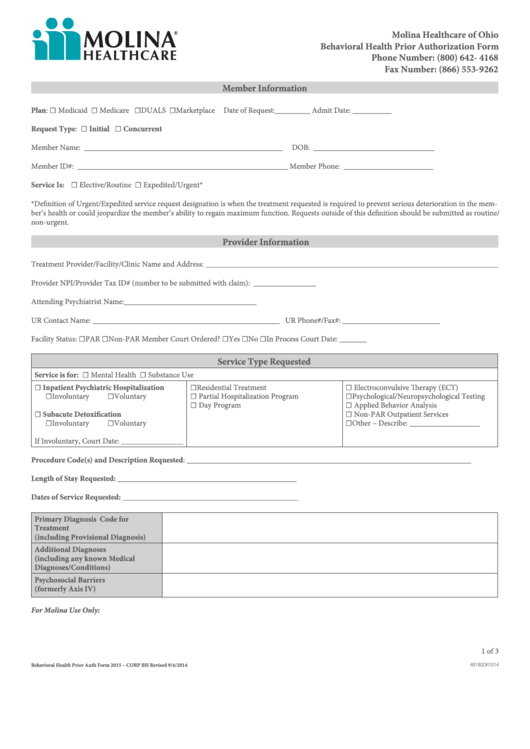
Fillable Molina Behavioral Health Prior Authorization Form Ohio
Prior authorization is when your provider gets approval from molina healthcare to provide you a service. • current (up to 6 months), adequate patient history related to the requested. 2023 medicaid pa guide/request form (vendors) effective 07.01.2023 important information for molina healthcare medicaid providers information generally required to support authorization decision making includes: Please use the “find a provider” tool.
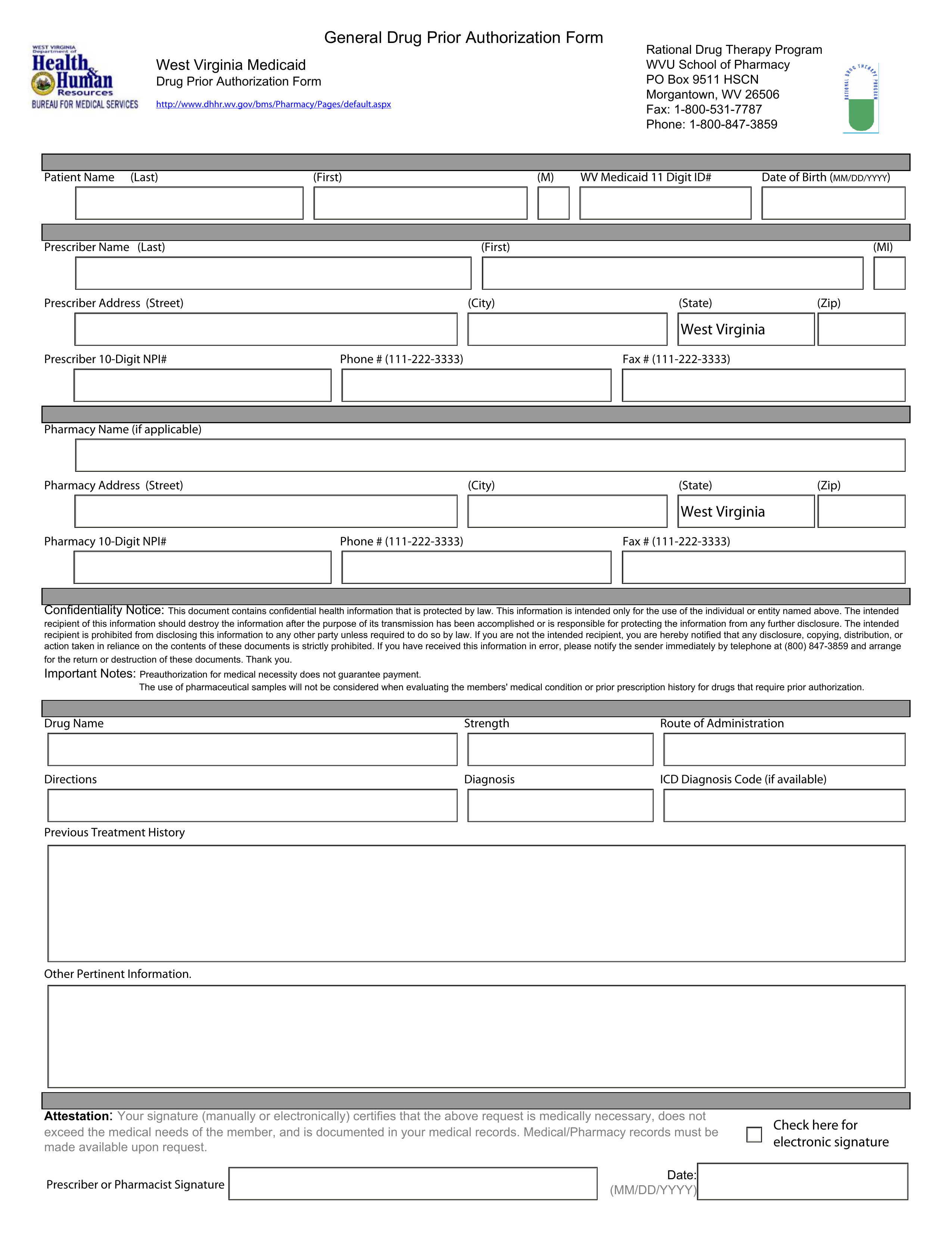
Free West Virginia Medicaid Prior (Rx) Authorization Form PDF
Add or close a location. Please use the “find a provider” tool above, which features pdf versions of our provider directories. The forms are also available on the frequently used forms page. Medicaid prior authorization annual review change log. Change in tax id and/or npi.
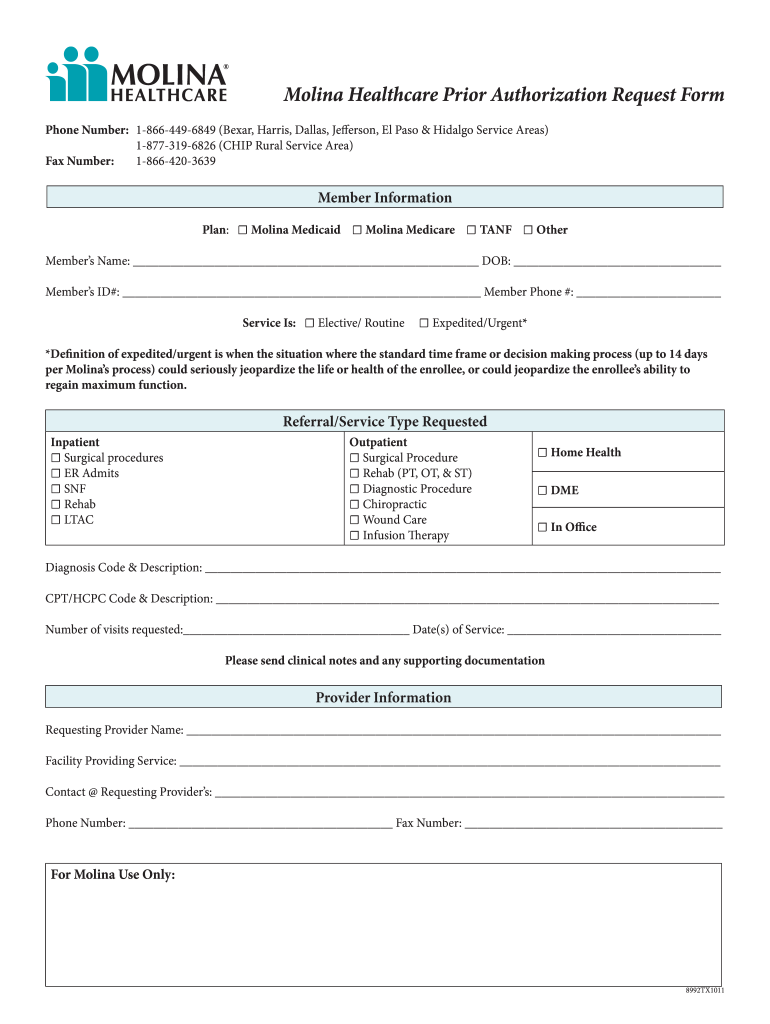
Molina Drug Prior Authorization Fill Online, Printable, Fillable
The forms are also available on the frequently used forms page. Medicaid prior authorization annual review change log. Medicaid prior authorization annual review report. We’ve provided the following resources to help you understand molina’s authorization process and obtain authorization for your patients when required. Please use the “find a provider” tool above, which features pdf versions of our provider directories.
UT Molina Healthcare Prior Authorization Form 20162022 Fill and Sign
The fastest route for prior authorization is submission via fax. Items on this list will only be dispensed after prior authorization from molina healthcare. Web change office location, hours, phone, fax, or email. Add or terminate a provider. Medicaid prior authorization annual review change log.
Molina Medicare Medication Prior Authorization Form Form Resume
Medicaid prior authorization annual review change log. Prior authorization is when your provider gets approval from molina healthcare to provide you a service. Items on this list will only be dispensed after prior authorization from molina healthcare. Please use the “find a provider” tool above, which features pdf versions of our provider directories. The forms are also available on the.
WA Molina Healthcare Behavioral Health Authorization/Notification Form
Medicaid prior authorization annual review report. The forms are also available on the frequently used forms page. Web getting care > prior authorizations prior authorizations what are prior authorizations? Please use the “find a provider” tool above, which features pdf versions of our provider directories. Web health insurance can be complicated—especially when it comes to authorizations.
Fill Free fillable Molina Healthcare Medicaid/Essential Plan Prior
• current (up to 6 months), adequate patient history related to the requested. Molina healthcare prior authorization request form and instructions. Add or terminate a provider. Prior authorization is when your provider gets approval from molina healthcare to provide you a service. Web health insurance can be complicated—especially when it comes to authorizations.
Molina Authorization Form Fill Online, Printable, Fillable, Blank
Medicaid prior authorization annual review change log. • current (up to 6 months), adequate patient history related to the requested. Web change office location, hours, phone, fax, or email. Please use the “find a provider” tool above, which features pdf versions of our provider directories. 2023 medicaid pa guide/request form (vendors) effective 07.01.2023 important information for molina healthcare medicaid providers.
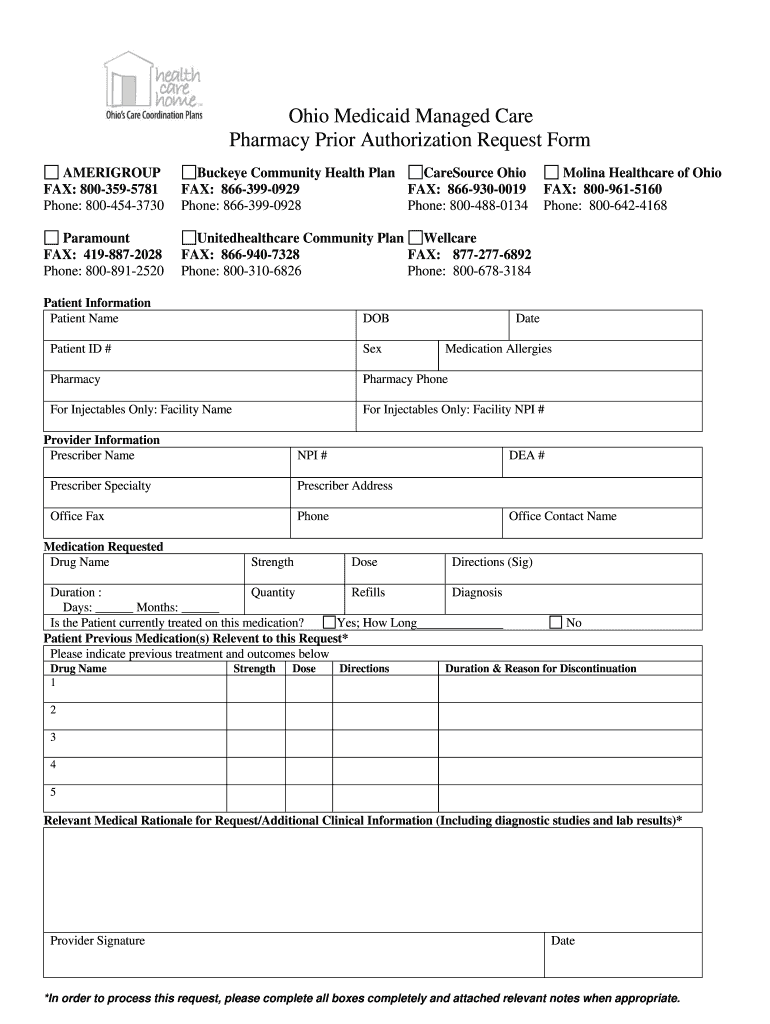
Ohio Medicaid Prior Authorization Form Fill Online, Printable
We’ve provided the following resources to help you understand molina’s authorization process and obtain authorization for your patients when required. Prior authorization is when your provider gets approval from molina healthcare to provide you a service. Web change office location, hours, phone, fax, or email. • current (up to 6 months), adequate patient history related to the requested. Medicaid prior.
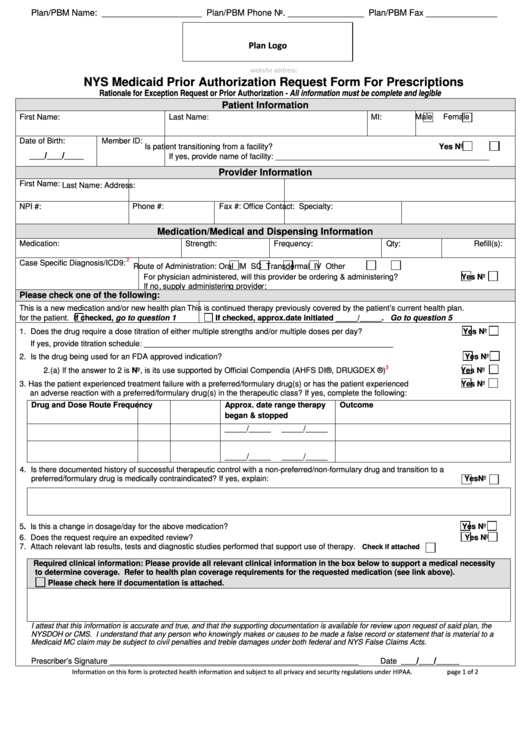
Fillable Nys Medicaid Prior Authorization Request Form For
Medicaid prior authorization annual review change log. Web change office location, hours, phone, fax, or email. Molina healthcare prior authorization request form and instructions. Add or close a location. The forms are also available on the frequently used forms page.
2023 Medicaid Pa Guide/Request Form (Vendors) Effective 07.01.2023 Important Information For Molina Healthcare Medicaid Providers Information Generally Required To Support Authorization Decision Making Includes:
Open or close your practice to new patients ( pcps only ). Web getting care > prior authorizations prior authorizations what are prior authorizations? Please use the “find a provider” tool above, which features pdf versions of our provider directories. Medicaid prior authorization annual review report.
Add Or Close A Location.
Add or terminate a provider. Change in tax id and/or npi. Web health insurance can be complicated—especially when it comes to authorizations. Prior authorization is when your provider gets approval from molina healthcare to provide you a service.
• Current (Up To 6 Months), Adequate Patient History Related To The Requested.
Items on this list will only be dispensed after prior authorization from molina healthcare. We’ve provided the following resources to help you understand molina’s authorization process and obtain authorization for your patients when required. Molina healthcare prior authorization request form and instructions. Web change office location, hours, phone, fax, or email.
The Forms Are Also Available On The Frequently Used Forms Page.
Medicaid prior authorization annual review change log. The fastest route for prior authorization is submission via fax.