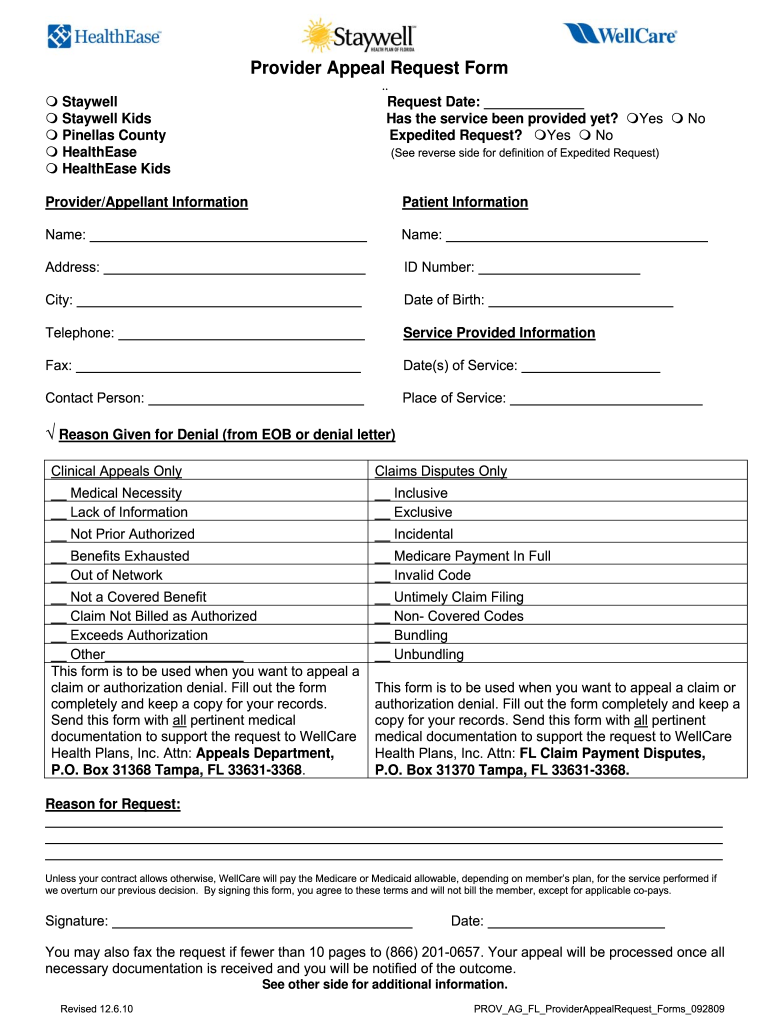
Wellcare Appeal Form
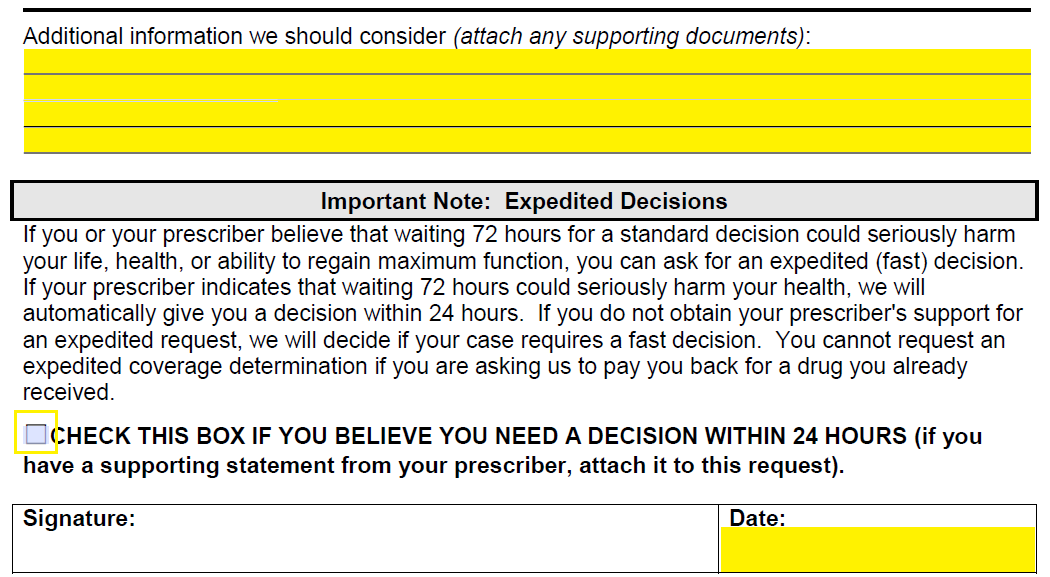
Wellcare Appeal Form - Wellcare, medicare pharmacy appeals, p.o. We have redesigned our website. Missouri care health plan attn: Web medication appeal request form you can use this form to request an appeal when a medication coverage determination request has been denied. How long do i have to submit an appeal? To access the form, please pick your state: Web request for redetermination of medicare prescription drug denial (appeal) (pdf) this form may be sent to us by mail or fax: Providers may file a written appeal with the missouri care complaints and appeals department. Complete an appeal of coverage determination request (pdf) and send it to: Send this form with all pertinent medical documentation to support the request to wellcare health plans, inc.
Do not attach original claim form.) Send this form with all pertinent medical documentation to support the request to wellcare health plans, inc. Complete an appeal of coverage determination request (pdf) and send it to: We have redesigned our website. Web request for redetermination of medicare prescription drug denial (appeal) (pdf) this form may be sent to us by mail or fax: An expedited redetermination (part d appeal) request can be made by phone at contact us or refer to the number on the back of your member id. Prior authorization request form (pdf) inpatient fax cover letter (pdf) medication appeal request form (pdf) medicaid drug coverage request form (pdf) notice of pregnancy form (pdf) provider incident report form (pdf) pcp change request form for prepaid health plans (phps) (pdf) Appeals 4205 philips farm road, suite 100 columbia, mo 65201. Please do not include this form with a corrected claim. Web claim” process in the wellcare by allwell provider manual, found on superiorhealthplan.com/providermanuals.
Contact us, or refer to the number on the back of your wellcare member id card. Web request for redetermination of medicare prescription drug denial (appeal) (pdf) this form may be sent to us by mail or fax: How long do i have to submit an appeal? Appeals should be addressed to: Do not attach original claim form.) We have redesigned our website. Refer to your medicare quick reference guide (qrg) for the appropriate phone number. You can now quickly request an appeal for your drug coverage through the request for redetermination form. Web claim” process in the wellcare by allwell provider manual, found on superiorhealthplan.com/providermanuals. Send this form with all pertinent medical documentation to support the request to wellcare health plans, inc.
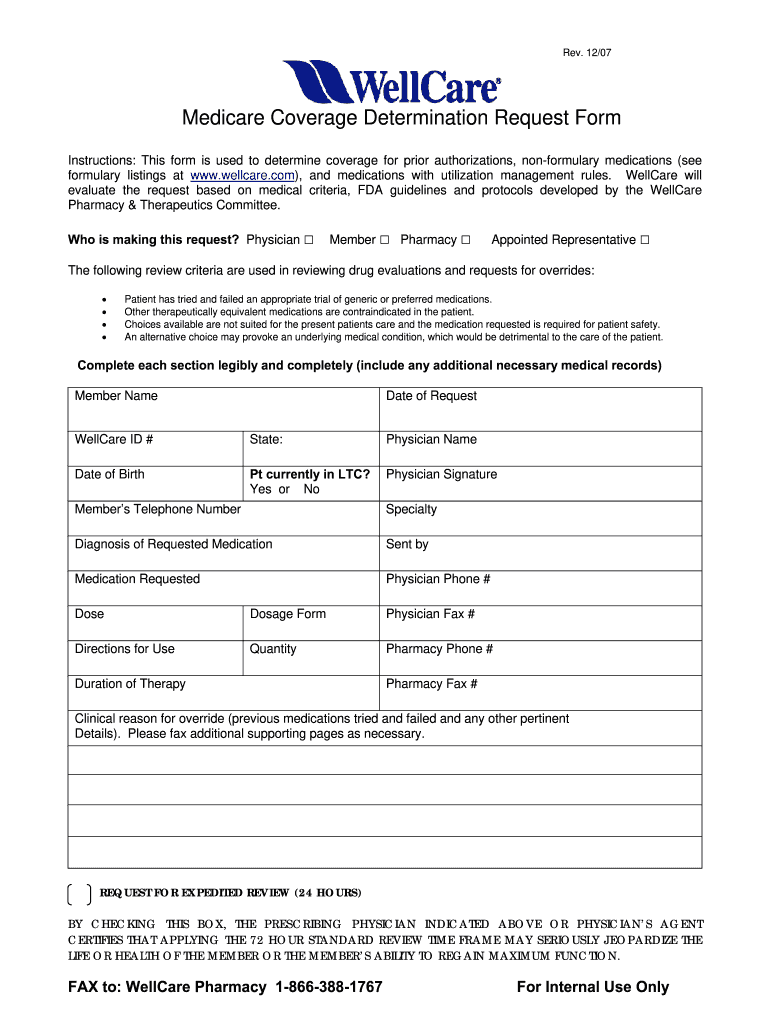
Free Wellcare Prior Prescription (Rx) Authorization Form PDF
Access key forms for authorizations, claims, pharmacy and more. Providers may file a written appeal with the missouri care complaints and appeals department. You can now quickly request an appeal for your drug coverage through the request for redetermination form. Web claim” process in the wellcare by allwell provider manual, found on superiorhealthplan.com/providermanuals. Web medication appeal request form you can.
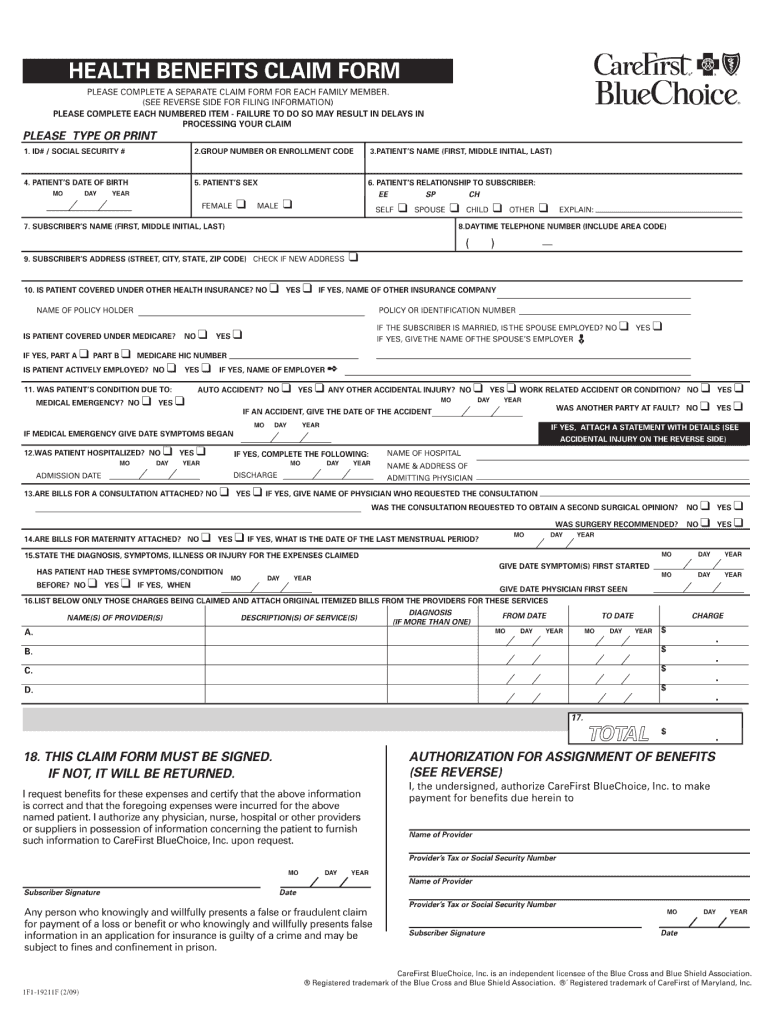
2009 Form CareFirst BlueChoice 1F119211F Fill Online, Printable
Send this form with all pertinent medical documentation to support the request to wellcare health plans, inc. Refer to your medicare quick reference guide (qrg) for the appropriate phone number. Providers may file a written appeal with the missouri care complaints and appeals department. Wellcare, medicare pharmacy appeals, p.o. Web medication appeal request form you can use this form to.
Free Wellcare Prior Prescription (Rx) Authorization Form PDF
Web claim” process in the wellcare by allwell provider manual, found on superiorhealthplan.com/providermanuals. You can now quickly request an appeal for your drug coverage through the request for redetermination form. Wellcare, medicare pharmacy appeals, p.o. Providers may file a written appeal with the missouri care complaints and appeals department. Please do not include this form with a corrected claim.
Wellcare Appeal Form Fill Online, Printable, Fillable, Blank pdfFiller
Web medication appeal request form you can use this form to request an appeal when a medication coverage determination request has been denied. Contact us, or refer to the number on the back of your wellcare member id card. How long do i have to submit an appeal? What is the procedure for filing an appeal? Web request for redetermination.
Wellcare Forms For Prior Authorization Fill Out and Sign Printable
Wellcare, medicare pharmacy appeals, p.o. Please do not include this form with a corrected claim. An expedited redetermination (part d appeal) request can be made by phone at contact us or refer to the number on the back of your member id. Providers may file a written appeal with the missouri care complaints and appeals department. How long do i.
Wellmed Prior Authorization Form Fill Online, Printable, Fillable
Appeals should be addressed to: Send this form with all pertinent medical documentation to support the request to wellcare health plans, inc. Web request for redetermination of medicare prescription drug denial (appeal) (pdf) this form may be sent to us by mail or fax: Missouri care health plan attn: Appeals 4205 philips farm road, suite 100 columbia, mo 65201.
Fillable Online Ohio Provider Medical Prior Authorization Request Form
Web request for redetermination of medicare prescription drug denial (appeal) (pdf) this form may be sent to us by mail or fax: Do not attach original claim form.) Web medication appeal request form you can use this form to request an appeal when a medication coverage determination request has been denied. Complete an appeal of coverage determination request (pdf) and.
Patient Portal Paloma Wellness and RehabPhysical Therapy
Prior authorization request form (pdf) inpatient fax cover letter (pdf) medication appeal request form (pdf) medicaid drug coverage request form (pdf) notice of pregnancy form (pdf) provider incident report form (pdf) pcp change request form for prepaid health plans (phps) (pdf) Web medication appeal request form you can use this form to request an appeal when a medication coverage determination.
WELLCARE HEALTH PLANS, INC. FORM 8K EX99.2 PRESENTATION DATED
Contact us, or refer to the number on the back of your wellcare member id card. Providers may file a written appeal with the missouri care complaints and appeals department. Access key forms for authorizations, claims, pharmacy and more. Refer to your medicare quick reference guide (qrg) for the appropriate phone number. Appeals should be addressed to:
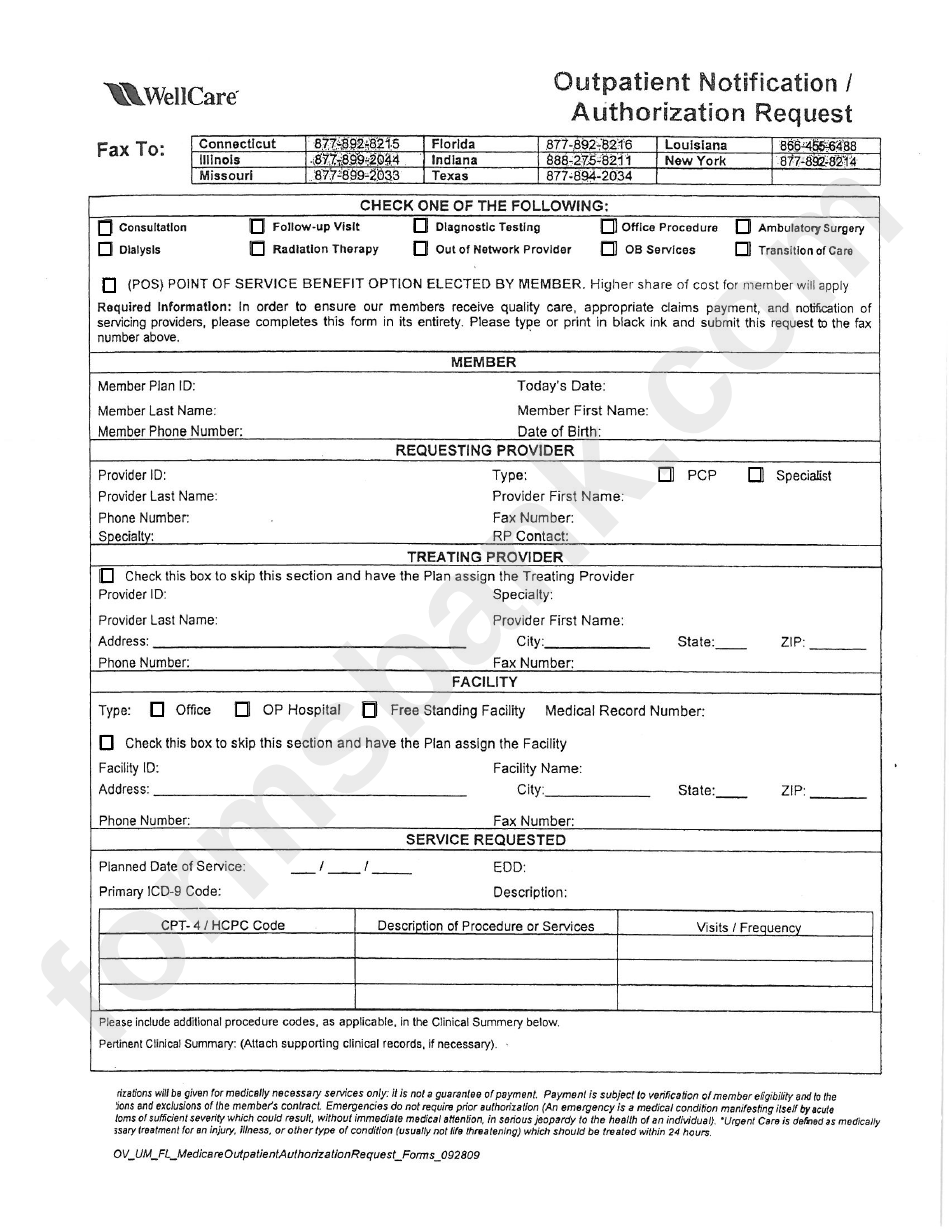
Fillable Outpatient Notification /authorization Request Wellcare
Please do not include this form with a corrected claim. Web medication appeal request form you can use this form to request an appeal when a medication coverage determination request has been denied. Do not attach original claim form.) Refer to your medicare quick reference guide (qrg) for the appropriate phone number. What is the procedure for filing an appeal?
Appeals Should Be Addressed To:
Web request for redetermination of medicare prescription drug denial (appeal) (pdf) this form may be sent to us by mail or fax: Please do not include this form with a corrected claim. Prior authorization request form (pdf) inpatient fax cover letter (pdf) medication appeal request form (pdf) medicaid drug coverage request form (pdf) notice of pregnancy form (pdf) provider incident report form (pdf) pcp change request form for prepaid health plans (phps) (pdf) Refer to your medicare quick reference guide (qrg) for the appropriate phone number.
You Can Now Quickly Request An Appeal For Your Drug Coverage Through The Request For Redetermination Form.
What is the procedure for filing an appeal? Send this form with all pertinent medical documentation to support the request to wellcare health plans, inc. Web claim” process in the wellcare by allwell provider manual, found on superiorhealthplan.com/providermanuals. Providers may file a written appeal with the missouri care complaints and appeals department.
Access Key Forms For Authorizations, Claims, Pharmacy And More.
To access the form, please pick your state: An expedited redetermination (part d appeal) request can be made by phone at contact us or refer to the number on the back of your member id. (attach medical records for code audits, code edits or authorization denials. How long do i have to submit an appeal?
Complete An Appeal Of Coverage Determination Request (Pdf) And Send It To:
Appeals 4205 philips farm road, suite 100 columbia, mo 65201. Web medication appeal request form you can use this form to request an appeal when a medication coverage determination request has been denied. Wellcare, medicare pharmacy appeals, p.o. Contact us, or refer to the number on the back of your wellcare member id card.